December 22, 2020

COVID-19’s Vexing Biological, Logistical and Political Vaccine Hurdles
Monday, December 14, 2020 will become an auspicious date in American history. The United States recorded its 300,000th COVID-19 death and set daily records for new COVID-19 cases (261,250) and hospitalizations (110,549). Disease spread is rampaging across all fifty states and shows no signs of slowing.
On this same day, COVID-19 nurse Sarah Lindsay received the first FDA-approved dosage of a coronavirus vaccine at Long Island Jewish Medical Center in Queens, New York. With that shot, America began its journey toward achieving COVID-19 herd immunity, ideally by mid-2021.
Achieving herd immunity in a short 6-to-8-month timespan will require nearly flawless vaccine development, production and distribution to a politically divided American populace. Each of these steps (vaccine development/approvals, manufacturing at scale and national distribution) is a monumental task in and of itself.
Engaging anti-vaxxers productively and combatting disinformation regarding COVID-19 vaccinations are essential to program success. Disinformation is spreading like wildfire on social media. More will come as variations in vaccine performance emerge and criminal elements peddle fake vaccines. Make no mistake. Disinformation and consumer exploitation pose material threats to widespread societal acceptance of COVID-19 vaccines.
Forewarned is forearmed. There are predictable biological, logistical and political hurdles that can occur in vaccine development, manufacturing and distribution. Anticipating and proactively addressing these hurdles will ease and speed the nation’s journey to defeat COVID-19.
Biological and Manufacturing Hurdles
Globally, there are over 400 coronavirus vaccines in clinical development. Approximately 75 are in clinical trials. The FDA has approved two, Pfizer’s and Moderna’s, for emergency usage. The rapid development and production of novel COVID-19 vaccines in less than a year is among the most compelling scientific achievements in human history. It is on par with sending a man to the moon and the Manhattan Project.
While administration of the Pfizer and Moderna vaccinations has begun, development and production of additional vaccines continues at warp speed. There remain, however, significant uncertainties regarding their development, production and approvals for emergency use.
All vaccines create molecules that trigger the body’s immune response to attack cells that mimic the targeted pathogen. When successful, that immunization process protects the body against infection from that natural pathogen. Once approximately 70% of a population carry protective antibodies, that population achieves “herd immunity” and the targeted pathogen (e.g. the coronavirus) ceases to be a public health threat.
Individual COVID-19 vaccines use different technologies to imitate the coronavirus’ antigens and trigger the body’s natural immune response. They fall into the following five categories.
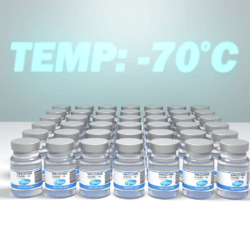
- Nucleic Acid Vaccines use DNA and RNA genetic material from the coronavirus to stimulate immune responses, including the production of antibodies. The now available Pfizer and Moderna vaccines are in this category. These novel vaccines use messenger-RNA to produce antigens (protein spikes) to induce an immune response. In phase III clinical trials, the Pfizer and Moderna vaccines were 95% effective in preventing the onset of COVID-19.
- Viral Vector Vaccines produce antigens using modified genetic material from the coronavirus. These noninfectious antigens trigger an immune response and antibody creation. The Ebola vaccine incorporated this technology. AstraZeneca’s and Johnson & Johnson’s COVID-19 vaccines also employ this technology and should become available early in 2021. Results from early-stage clinical trials suggest the AstraZeneca vaccine is 60% to 90% effective in provoking a positive immune response.
- Protein Subunit Vaccines contain purified pieces of coronavirus proteins selected for their ability to create noninfectious antigens that stimulate an immune response and antibody creation. These types of vaccines are in widespread use (e.g. to prevent Hepatitis B), employ a well-established technology, are low cost and very safe. The Novavax and Sanofi vaccines employ this technology and should become available by mid-2021.
- Multitope Peptide Vaccines are a subset of Protein Subunit Vaccines. Peptides are smaller than proteins and chemically synthesized. Multitope (or targeting multiple parts of the virus) peptide vaccines stimulate immune response with synthetic peptide immunogens. Use of synthetic peptides is cost-effective and very safe. The COVAXX vaccine employs this technology and should become available by mid-2021.
(Please note the author served on COVAXX’s Vaccine Prioritization Advisory Group) - Whole Virus Vaccines inject weakened or inactivated coronavirus particles into the bloodstream to trigger an immune response and antibody creation. Most vaccines historically have used this technology. A number of these inactivated Whole Virus Vaccines are under development in China.
In addition to creating effective vaccines, several pharma companies have began manufacturing vaccines at industrial scale to speed their time to market. Through Operation Warp Speed, the U.S. has committed to buy as many as 1.5 billion vaccine doses from Pfizer, Moderna, AstraZeneca, Johnson & Johnson, Novavax and Sanofi at prices between $3-4 (AstraZeneca) and $32-37 (Moderna) per dose.
Despite or perhaps because of the remarkable scientific advances, there are significant variations in the timing, efficacy, delivery mechanics, storage requirements, immunity duration and side effects of the five vaccine types.
Moreover, science still has much to learn about the vaccines. Unanswered questions include the durability of the immunity they provide, their ability to limit transmission as well as prevent disease and their potential to trigger allergic shocks in susceptible populations.
Typically, public health officials use a mix and match approach to formulating vaccines so that recipients are indifferent regarding which vaccine they receive. That will not be possible as COVID-19 manufacturers rush vaccines to market upon FDA approvals. Given their diversity and the speed with which they are coming to market, there will be significant variations in the different vaccines’ relative performance.
Logistical and Political Hurdles
Unfortunately, development and manufacturing of COVID-19 vaccines without adequate national distribution is a recipe for failure. Distributing these vaccines to hundreds of millions of Americans is a logistical challenge equivalent of D-Day, building the space station and “Hands Across America” all rolled into one.
Ineffective vaccine distribution within some segments of the population is possible, perhaps probable, because of misinformation, unforeseen adverse events and/or entrenched anti-vaxxer beliefs. To the extent that vaccine distribution underperforms with select populations, it will increase COVID-19’s disease and death toll among those populations.
Achieving herd immunity against COVID-19 will require roughly 70% of U.S. adults to receive voluntary vaccinations. This is a tall order. Only 43% of U.S. adults received influenza vaccines in 2019. That was the highest vaccination rate in the last decade. Moreover, there was wide variation among states and between ethnic groups.
As in all public health matters, states will take the lead in vaccine prioritization and distribution with guidance from the federal government. On the plus side, a Marist Poll from early December indicates that 61% of Americans will take a COVID-19 vaccine, up from 49% in September.
Even with this positive trend, many Americans remain unwilling to embrace COVID-19 vaccinations. A significant percentage of these reluctant Americans are persuadable with appropriate public health messaging. However, a sizable anti-vaxxer segment of the American is adamant in their opposition. It is imperative not to underestimate the difficulty in getting these individuals to reverse deeply held beliefs.
Social media amplifies the noise and confusion surrounding the public’s understanding of vaccinations.
Wild theories about COVID-19 vaccinations abound. One currently gaining traction asserts that the government or Bill Gates is using fake vaccine shots to implant location devices.
Understanding and addressing “the pictures” inside the heads of anti-vaxxers is prerequisite for increasing their participation in a national vaccination campaign. Traditional public health approaches are unlikely to work. There needs to be different and a more effective form of discourse.
Creative marketing approaches can work. The Texas Department of Transportation dramatically reduced roadside trash beginning in 1986 with the launch of its “Don’t Mess with Texas” campaign. Along the same lines, it’s time to “Stick It to COVID-19!™” by engaging the nation’s best marketing minds in the mother-of-all campaigns to get as many Americans as possible vaccinated against COVID-19.
Conclusion: Bridging the Political Divide Through COVID-19 Vaccinations
December 14th also was the day that the Electoral College certified Joe Biden’s election as the next President of the United States. This certification came amid an unprecedented attack by a sitting President on the electoral process. President Trump has used his bully pulpit and filed almost sixty unsuccessful lawsuits to challenge election results. Reflecting this political turmoil, only 62% of Americans believe Biden won the presidential election fairly.
Undoubtedly, there is significant overlap between anti-vaxxers and those believing Biden stole the election from President Trump. Grievance politics feed on insecurity and nurture conspiracy theories.
Many who spurn COVID-19 vaccines and support Trump are ignoring the Trump administration’s leadership in speeding vaccine development through Project Warp Speed. Linking Trump to vaccine distribution through creative messaging may help persuade some anti-vaxxers.
Additionally, segments of the African American and Latino communities are also highly skeptical of vaccine programs. Public health leaders must address the specific concerns of these communities to advance widespread vaccinations against COVID-19.
Achieving COVID-19 herd immunity requires winning the hearts, minds and trust of numerous anti-vaxxers of all persuasions. It won’t be easy, but it is not impossible. Credit Vice President Pence, Karen Pence, President-elect Biden, Jill Biden, House Speaker Nancy Pelosi, Senate Majority Leader Mitch McConnell and Surgeon General Jerome Adams for receiving COVID-19 vaccinations on live television. Every positive message helps discredit disinformation campaigns.
The nation’s march to herd immunity must overcome inherent vaccine differences, massive manufacturing and distribution challenges and a polarized political environment. Failure isn’t a viable option. It would further deepen distrust and division.
Alternatively, eliminating COVID-19 in the next 6-8 months will enable American society to reopen, the American people to reengage with one another and the American economy to thrive. With a shared sense of purpose, an all-American success could even increase trust in public institutions and improve societal discourse.
The COVID-19 pandemic is testing whether the United States, as currently configured and operating, can come together to defeat a microscopic virus that is weakening the nation’s health, prosperity and confidence. The next 6-8 months are pivotal. For better or worse, America’s collective effort in combatting COVID-19 will shape the nation’s health and its political character for the foreseeable future.
 Get more on the vaccine rollout in the new 4sight Health Roundup
Get more on the vaccine rollout in the new 4sight Health Roundup
Listen to the 4sight Health Roundup, a Friday podcast where David Burda interviews Dave Johnson and Julie Murchinson about the week’s hot topics. Recent episodes cover different angles of the rapidly changing vaccine situation.
Subscribe on iTunes, Spotify, other services.