April 5, 2022

Cracks in the Foundation (Part 3): Overcoming Healthcare’s Services-Need Mismatch
Editor’s note: This piece is the third in a series of six columns in which David Johnson addresses five structural defects undermining nonprofit healthcare. He outlined all five defects in the first column of the series. Part two is here.
At the top of my reading list last summer was The Hospital: Life, Death and Dollars in a Small American Town by Brian Alexander. I expected Alexander’s book to portray the ups and downs of a rural hospital fighting for survival. It does that superbly.
Surprisingly, The Hospital also chronicles the daily travails of local residents seeking vital care services they desperately need. Among them is Keith Swihart, an affable, hard-working, heavyset man who struggles to care for a special-needs son, afford insulin and ward off medical bill collectors. Diabetes ultimately costs Keith his right foot and most of his eyesight. Only 39, Keith hobbles to endless medical appointments and treatments. An effective diabetes management program could have kept Keith active and productive. Instead, as he spirals downhill, American society funds Keith’s enormous treatment and disability costs. What a monumental and preventable tragedy.
Healthcare’s Profound Services-Need Mismatch
There are countless Keith Swiharts living in America, especially in low-income urban and rural communities. U.S. healthcare is not providing them with the basic care services they need to lead longer, healthier and happier lives. Inadequate access to coordinated social and healthcare services underlies expansive differences in life expectancy, exceeding 20 years between wealthy and poor communities. Despite medical advances, U.S. life expectancy has declined consistently on both an absolute and relative basis since 2014.[1]
By the early 1990s, sedentary lifestyles, greater portion sizes and processed food consumption had triggered massive increases in obesity and related chronic conditions. In response, the Centers for Disease Control (CDC) added “Prevention” to its name in 1992. Even with more preventive care, the CDC estimated in 2020 that, as of 2018, more than 42% of U.S. adults were obese.[2] Meanwhile, chronic disease and mental health conditions account for 90% of the nation’s healthcare expenditure.[3] It doesn’t have to be this way. Providers are ideally positioned to engage and help Americans improve their well-being and to promote healthier communities.
Elevating health promotion to equal status with disease treatment, however, runs counter to medical practice, culture and economics. Overcoming legacy behaviors and attitudes will require full-throttled commitments to improving social determinants of health.
Health Multipliers
The antiseptic phrase social determinants of health mechanically captures the immense importance of education, housing, food security, transportation and other social factors in promoting well-being and enhancing human potential. But the words fail to stir the blood.
“Social” as a modifier of “determinants” is far too limiting. The exhibit below displays the numerous and complex interconnections that foster longer, healthier lives. It shows that social and economic factors, health behaviors and the physical environment drive 80% of health outcomes in theUnited States. Yet America disproportionately invests its healthcare resources in clinical care, which accounts for only 20% of outcomes. More of the same investments will only yield more of the same dismal health outcomes.
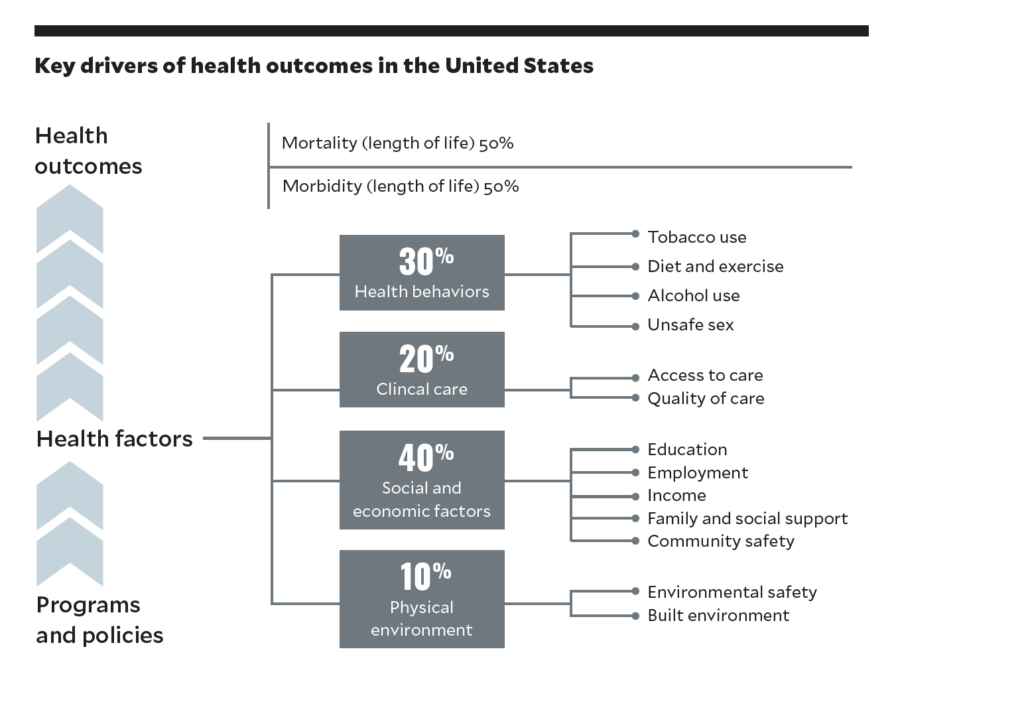
Source: University of Wisconsin Population Health Institute, “What works for health: evidence for decision-making,” 2014
By contrast, enhancing social determinants can catapult disadvantaged individuals and communities into sustained well-being and higher productivity. The terminology describing these transformative investments should capture its inherent vigor and enormous potential.
A descriptor superior to social determinants of health is healthy multipliers. It is clean, active and progressive, describing the real initiatives — i.e., the multipliers — that embody the essence of what’s required for healthy living.
The idea of healthy multipliers also represents the strategic shift that health systems must make to combat the nation’s chronic disease pandemic. Former Cleveland Clinic CEO Toby Cosgrove observed that “the state of our nation depends on the state of our health.” For the nation to prosper, America must become healthier. As is happening in Philadelphia, that requires health systems to promote communitywide health through targeted initiatives.
Pivoting to Healthy Multipliers
Stephen Klasko, MD, former CEO of Jefferson Health in Philadelphia, believes health systems “shouldn’t be limited by the natural order of things.” So he approaches strategic planning in a novel way. He looks ahead 10 years, imagines a desired future and works to achieve it. Translating his beliefs into actions, Klasko reset Jefferson’s strategy in 2017 by “placing health equity at the center of everything we do.” Leading by example, Klasko linked 25% of his incentive compensation to reducing health inequities.[4]
Jefferson Health then took the following concrete steps, among others, to improve health status in Philadelphia’s low-income communities:
- Established the Philadelphia Collaborative for Health Equity
- Partnered with Temple to reduce disparities in stroke outcomes
- Partnered with Novartis to reduce disparities in cardiovascular diseases
- Launched #realtalk to promote COVID vaccinations in African American communities
These initiatives are healthy multipliers in action. Outcomes matter. Jefferson funds digital health companies that make a real difference in promoting health equity. As Klasko recently commented: “‥. it’s about getting rid of food deserts by drone-delivering food or using community health partners to really help the 5% of people who end up using 50% of the resources.”
Health systems are complex organizations with expansive investments in facilities, labor and technology. As Jefferson Health illustrates, embracing healthier outcomes, equity and well-being is liberating. It enables health systems to engage productively with their communities.
Absent this commitment, the yawning services-need gap will widen, health disparities will increase and the state of the nation’s health will worsen. Embracing health as an organizational imperative is clarifying. It’s what management guru Peter Drucker meant when distinguishing between “doing things right” and “doing the right thing.”
Doing the right thing requires health systems to make absolute commitments to putting consumers’ interests first. Those that do so will gain market relevance. Those that don’t will lose it.
Let’s apply “Klaskoian” logic to health systems’ current reality. Healthy multipliers will gain increasing importance during the next 10 years. Doesn’t it make strategic sense to invest in them now? The answer is beyond obvious.
Checklist for Remedying the Services-Need Mismatch
Here are seven strategic steps health systems can undertake to overcome services-need mismatches:
- Document and measure care gaps.
- Make consumers’ health and well-being the organizational priority.
- Understand the cultural dynamics linking poverty and poor health.
- Partner with like-minded organizations to promote healthier communities.
- Prioritize holistic primary care, preventive and mental health services.
- Address disparities in healthcare outcomes.
- Invest expansively in healthy multipliers.
HFMA published this series “Cracks in the Foundation” February – July 2022.
- Cracks in the Foundation — 5 Structural Defects Are Undermining Nonprofit Healthcare Part 1
- Part 2: Overcoming Healthcare’s Artificial Economics
- Part 3: Overcoming Healthcare’s Services-Need Mismatch
- Part 4: Overcoming U.S. Health Systems’ Brittle Business Model
- Part 5: Overcoming Regulatory Headwinds
- Part 6: Overcoming Inadequate Leadership
Sources
- Venkataramani, A.S., O’Brien, R., and Tsai, A.C., “Declining life expectancy in the United States: The need for social policy as health policy,” JAMA Network, Feb. 16, 2021.
- Hales, C.M., Carroll, M.D., Fryar, C.D., and Ogden, C.L., “Prevalence of obesity and severe obesity among adults: United States, 2017–2018,” CDC National Center of Health Statistics, NDHS data brief, February 2020.
- National Center for Chronic Disease Prevention and Health Promotion, “Health and economic costs of chronic diseases,” CDC, page last reviewed March 9, 2022
- Advisory Board, “Steve Klasko on diverging from the ‘natural order of things’ to move health care forward,” Daily Briefing, Nov. 2, 2022