- Have the courage to lead revolutionary transformation.
- Streamline organizational governance.
- Determine and articulate the “just cause” that will guide organizational strategy.
- Undertake comprehensive culture change to educate and engage employees.
- Tap the community for support and inspiration.
- Remember that sacred cows make the best hamburger.
- Start yesterday.
July 28, 2022
Cracks in the Foundation (Part 6): Overcoming Inadequate Leadership
Nobody likes getting ripped off. I had that experience on a recent trip to Boston, when Avis charged me a $6 service fee for the “convenience” of paying a $2 cashless toll. Avis usually lives up to its “We try harder” mantra, but this experience left a bad taste. Consumers can have a similar experience with hospital prices and economics.
The American Hospital Association’s (AHA) April 2022 Cost of Caring report pleads for more funding to offset double-digit increases in labor, supply and drug costs. Meanwhile, the latest West Health-Gallup Healthcare Value Index found that 95% of American adults find the perceived value of the healthcare they receive is “inconsistent” or “poor.” Healthcare’s leaders, including board leadership, should sit up and take notice.
A Failure of Healthcare Leadership
The economic principle is not complicated and applies to all industries. Demanding more money for overpriced services is no way to win consumers’ hearts, minds and wallets. Warren Buffett famously observed, “Price is what you pay. Value is what you get.”
It should be immediately clear to healthcare leaders that the disconnect between prices paid and value received is at the heart of our industry’s dysfunction. Like Avis, health systems need to “try harder” to improve care access, outcomes and affordability.
During COVID-19, the proverbial chickens have come home to roost. The healthcare system’s structural imbalances were obvious and catastrophic. Hospitals required a government bailout while big insurance and big pharma reaped huge profits. Emerging from COVID, hospitals confront an existential threat. Doubling down on existing business models, as the AHA advocates, increases both strategic and financial risk.
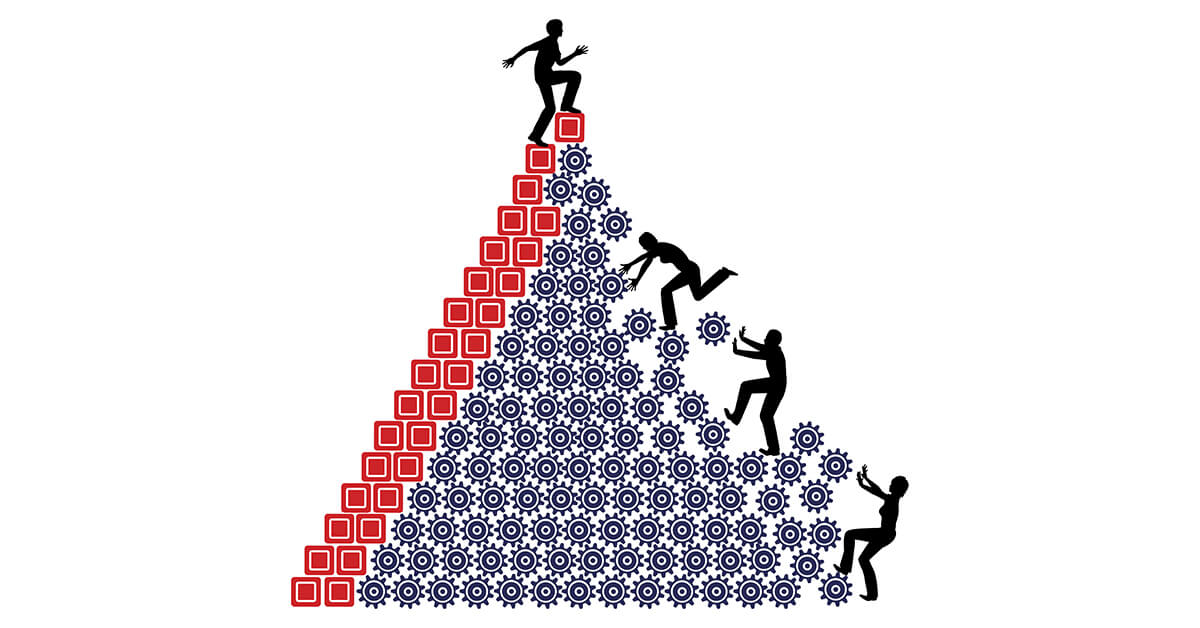
As a consequence, it’s time for health system leaders to reject volume-based business models and embrace value-driven care delivery. To fix healthcare, they must right-size care delivery, promote health, improve customer experience and deliver the highest-quality care outcomes at the lowest cost. This shift requires courageous leadership, which is unfortunately in short supply, to make the necessary changes.
Yet they must: It has never been more necessary for all leaders to recognize that the value quest is enduring and just. It optimizes individual and community well-being without breaking the bank. Success requires vision, courageous leadership and major structural reforms. Improving governance within nonprofit health systems will speed the nation’s journey toward consistent delivery of kinder, smarter and affordable care for all Americans.
The Conundrum of Nonprofit Healthcare’s Board Leadership
Nonprofits dominate U.S. care delivery. Their boards tend to be large, volunteer, philanthropic and lacking in needed expertise. Like volunteer boards for museums and cultural institutions, they exist primarily to support and sustain institutional longevity. Nonprofit health system boards all too often lack the business acumen to navigate their large, complex organizations through healthcare’s dynamic and disruptive marketplace.
Compounding the challenge, these health systems have misaligned management and board incentives. Given their tax-exempt status, the nonprofits cannot grant equity. Board members receive limited or no compensation. Management teams typically work under short-term contracts that incentivize near-term performance, not long-term sustainability.
Consequently, nonprofit health system boards tend to be strategically defensive, supportive of status-quo business practices and reliant on management for organizational strategy. They rarely pursue transformative repositioning. Instead, most give lip service to value creation while pursuing status quo business practices.
Given healthcare’s turbulent operating environment, these organizations must become more responsive to customer and community needs. Likewise, their boards must become more proactive in setting strategy and establishing greater accountability for organizational performance and community wellbeing.
These are no small tasks. Accomplishing them requires inspired leadership.
Reimagining Leadership
To improve organizational decision-making and risk management, nonprofit health systems must change their governance structure in six key ways:
- Vest governance and long-term strategy in a single, relatively small board (no more than 15 members) with appropriate sub-committees and quarterly meetings.
- Compensate board members for their time and expertise.
- Recruit board members with diverse backgrounds and experience.
- Include a strong community voice in organizational governance.
- Emphasize cultural reengineering and employee empowerment.
- Align performance metrics and management compensation with organizational strategy.
Transforming health system governance is easy compared with rewiring culture, engaging consumers, inspiring employees and operationalizing transformation. America cannot attain the healthcare system its people deserve without full commitment to value creation. This type of commitment is exemplified by the two leaders’ stories in the sidebar below.
Transformation must come from within. Healthcare’s leaders must be equal to the task or risk losing control of their organizations’ destinies. The clock is ticking.
7 Strategies for Health Systems to Apply
Here are seven strategies that health systems can apply to create inspired leadership for advancing transformative change:
2 Stories of Courageous Leadership
James Merlino, MD and David Feinberg, MD, MBA led organization-wide efforts at the Cleveland Clinic and UCLA Medical Center respectively to recenter care delivery on patients.
In 2005, Merlino left the Clinic, believing it “was an evil place that treated patients poorly and fostered an environment in which people did not work together or support one another.” Five years later, he returned as its chief clinical transformation officer.
In his book Service Fanatics: How to Build Superior Patient Experience the Cleveland Clinic Way, Merlino describes the clinic’s massive, multiyear program to create an organizational culture centered on patient experience. Merlino’s team produced a training video on patient empathy that captures their program’s essence and spirit. The video went viral and touched millions.
The program engaged all employees in multiple sessions. Its goal was making the Clinic’s “Patients First” motto a reality. Patient care needed to become as important as medical cures.
When David Feinberg became UCLA’s CEO in 2007, he began doing patient rounds. As he describes in a 2011 TedXTalk, Feinberg discovered cold food, dirty rooms, excessive wait times, disengaged employees and neglected patients. He synthesized UCLA’s attitude regarding patients as “Aren’t you lucky to see us.”
Like Merlino, Feinberg got back to the basics and reengineered a broken culture. Programming centered on service improvement and patient engagement. In the process, employee attitudes toward patients shifted from indifference to asking, “How can I help.”
Both Cleveland Clinic and UCLA saw their patient satisfaction scores skyrocket. Relentless focus on patient experience pays enormous dividends. Enthusiastic and active employees drove implementation. Engaged employees are healthcare’s secret weapon for transforming broken business models, but they need inspired leadership to work their magic.
As hard as it was to change institutional cultures within the Cleveland Clinic and UCLA, decentralizing care delivery to promote communitywide health will be much harder. Healthcare’s elevation of treatment over prevention rests on decades of entrenched behaviors and perverse economic incentives. Building new cultures based on value and well-being will take long, sustained and heroic effort.
HFMA published this series “Cracks in the Foundation” February – July 2022.
- Cracks in the Foundation — 5 Structural Defects Are Undermining Nonprofit Healthcare Part 1
- Part 2: Overcoming Healthcare’s Artificial Economics
- Part 3: Overcoming Healthcare’s Services-Need Mismatch
- Part 4: Overcoming U.S. Health Systems’ Brittle Business Model
- Part 5: Overcoming Regulatory Headwinds
- Part 6: Overcoming Inadequate Leadership





