July 21, 2015
Crossing the Technology Chasm: Tele-ICUs Save Lives and Money
Crossing the Technology Chasm: Tele-ICUs Save Lives and Money
The Leapfrog Group’s[1] fact sheet on ICU Physician Staffing estimates that preventable ICU deaths exceed 54,000 each year. This figure excludes “adverse events” that cause harm without death and lead to costly additional care. Despite critical care’s complexity, hospitals can dramatically reduce ICU deaths and care costs with enhanced staffing, technology and protocols.
Tele-ICUs centralize critical care management in 24/7 “command centers” that treat patients in multiple hospitals. Mortality, length of stay and the costs plummet. Tele-ICUs have existed since 2000, but have struggled to achieve critical mass. The obstacles are principally human. Fortunately, disruptive innovation emerges to displace entrenched and inefficient businesses. Expect Tele-ICUs to cross the “technology chasm” as hospitals invest to provide a higher standard of care. Transforming critical care through Tele-ICUs illustrates health reform’s potential to standardize excellence through superior application of labor and technology.
Critical Care’s Critical Importance
Critical care is high-stakes medicine, operating where life meets death. ICUs have hospitals’ highest mortality rates and can consume almost forty percent of costs.[2] ICUs are complex, high-risk environments that require caregivers to filter data continuously and act instantly. Superior critical care requires accurate diagnoses and timely treatments. Intensivists, physicians who specialize in treating intensive care patients, are essential to achieving superior ICU outcomes. The Leapfrog Group informs Americans on hospital safety and quality. Their research finds ICUs managed or co-managed by intensivists have forty-percent-lower mortality. Unfortunately, the lack of standardization, a shortage of intensivists and entrenched physician behaviors (e.g. not addressing patient distress until physically present in the ICU) lead to frequent, predictable ICU treatment errors (e.g. not taking patients off ventilators at the optimum time). Driven by demographics and exploding chronic disease, increasing numbers of sicker ICU patients are compounding ICU service demands. The status quo will not hold.
Tele-ICUs’ Promise
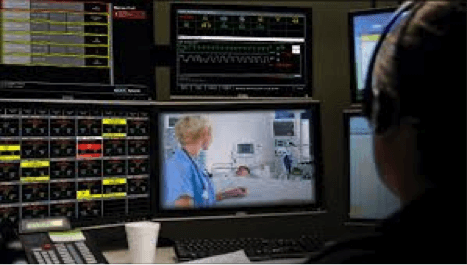
Tele-ICUs centralize critical care monitoring, consultation and care services. High resolutions screens enable intensivists to communicate and coordinate care delivery with patients and on-site caregivers. Control-center intensivists monitor up to 100 ICU patients, a ten-fold productivity increase over on-site intensivists. Tele-ICUs standardize evidenced-based protocols, build on experience and reduce transfers. Patients receive better care closer to home. Patient satisfaction, outcomes and caregiver morale improve while costs decline.
The University of Massachusetts Memorial Medical Center (UMMMC) participated in a study that contrasted the performance of its Tele-ICUs with its in-hospital ICU. The compelling results of the Tele-ICU’s performance included:[3]
- Twenty percent lower ICU mortality despite a significant increase in patient severity
- Two-day lower length of stay
- One-year payback for the $7.1 million installation cost
- $2600 decline in cost-per-case
Extrapolating across Massachusetts, the study estimated that statewide adoption of Tele-ICUs would save 350 lives annually and generate payer savings exceeding $122 million.
Crossing the Technology Chasm
In his seminal marketing book, Crossing the Chasm, Geoffrey Moore identifies an “adoption chasm” that emerges as disruptive technologies expand their marketing beyond “early adopters” (enthusiasts and visionaries) to “early majority” buyers (pragmatists).
As a disruptive technology approaches fifteen percent market share, it confronts a “tipping point” marketing challenge. Companies must convince cautious “mainstream” buyers of their technology’s long-term sustainability.
ICUs managed or co-managed with intensivists now operate in roughly twelve percent of America’s hospitals.[4] Given their short supply, staffing on-site ICUs with intensivists is difficult and expensive. Tele-ICUs offer the same or better outcomes at lower costs. As a result, Tele-ICU’s are approaching Moore’s adoption chasm and will cross it by meeting Leapfrog’s standard for critical care more efficiently than on-site ICUs. The current payment system has slowed adoption by reimbursing treatment activity rather than treatment outcomes. Movement to “value-based” payments will accelerate Tele-ICU adoption.
The Trailblazer and the Colonel
BMO partners with Fortune Magazine to spotlight “trailblazers,” young-company entrepreneurs employing disruption to change business or consumer behavior. As CEO of Advanced ICU Care, Dr. Mary Jo Gorman is a trailblazer pushing Tele-ICU’s disruptive technology into the critical care mainstream.
Advanced ICU Care manages ICUs for almost forty hospitals with 600 ICU beds in thirteen states from a command center in St. Louis. It is the nation’s largest Tele-ICU company. It employs the widely-used Phillips ICU software and focuses on mid-size hospitals lacking resources to launch their own Tele-ICU programs. Gorman’s team works in concert with local caregivers to confirm diagnoses and apply standardized care across the company’s patient population. She believes in rigorous benchmarking and data transparency. A 2010 study of 10,000 ICU patients (5397 with Advanced ICU Care; 4612 control group) yielded the following results:
- 40% lower mortality
- 25% lower length of stay
- 17% more ICU cases (by avoiding transfer and receiving treatment at local hospital)
In the just finished second quarter, Advanced ICU Care treated 7,417 critical care patients across its network. The company saved 313 hospital lives, including 178 ICU lives. Effective treatment saved 13,953 hospital days, including 4,862 ICU days[5].
![]() Dr. Greg Beilman worked in Iraq with General Brian Gamble and General David Petraeus to revolutionize treatment protocols for wounded soldiers. Roughly a quarter of wounded soldiers died from WWII through the First Gulf War. Their innovative triaging has reduced mortality below ten percent. The key breakthrough was providing appropriate care at battlefront, regional and U.S. treatment facilities. Severely wounded soldiers received care at better-equipped hospitals. Upon returning to the University of Minnesota and Fairview Health Services, Dr. Beilman employed military-tested concepts of standardization, teamwork, data transparency and two-way communication to launch a system-wide Tele-ICU at Fairview’s hospitals. The mission was clear: focus on improving each patient’s ICU care. This short video shows how Fairview’s Tele-ICU interaction works.
Dr. Greg Beilman worked in Iraq with General Brian Gamble and General David Petraeus to revolutionize treatment protocols for wounded soldiers. Roughly a quarter of wounded soldiers died from WWII through the First Gulf War. Their innovative triaging has reduced mortality below ten percent. The key breakthrough was providing appropriate care at battlefront, regional and U.S. treatment facilities. Severely wounded soldiers received care at better-equipped hospitals. Upon returning to the University of Minnesota and Fairview Health Services, Dr. Beilman employed military-tested concepts of standardization, teamwork, data transparency and two-way communication to launch a system-wide Tele-ICU at Fairview’s hospitals. The mission was clear: focus on improving each patient’s ICU care. This short video shows how Fairview’s Tele-ICU interaction works.
Like Advanced ICU Care, Fairview’s intensivists manage ICUs throughout their network. Unlike Advanced ICU Care, Fairview employs its own electronic medical records (run on Epic software) to track patient status. Fairview’s Tele-ICU bridges its academic and community practices to deliver better ICU care closer to home. Fairview locates its 24/7 command center at the University of Minnesota Medical Center (UMMC). On-duty intensivists assist residents in UMMC’s ICU, which improves both care delivery and medical education. On its one-year anniversary, Fairview issued a report card that chronicles improvement in ICU care coordination, mortality and outcomes. It contains a small graphic with the caption “Together we achieve more!”
Tele-ICUs and the Power of Market-Based Reform
Tele-ICUs disruptive use of labor and technology delivers superior outcomes at lower costs. They have established a higher standard for critical care delivery. Hospitals have been slow to adopt this higher care standard. Earlier this month, Asiana Flight 214 crashed in San Francisco. The public’s reaction, news coverage and official commentary underscore America’s zero tolerance for airplane failure. The airline industry will study this accident, learn from it and adjust operations/regulations to prevent its reoccurrence. Healthcare can learn from the airline industry’s full commitment to safety and quality. Too much performance variation and inconsistent performance measurement cause unnecessary death and harm in America’s ICU’s. Advanced ICU Care and Fairview are demonstrating that employing disruptive innovation in critical care save lives and money. Their success illustrates the power of market-based reform to transform healthcare delivery.
[1] The Leapfrog Group is a non-profit organization funded by large employers that has the following three aims: inform Americans about health and safety; promote full public disclosure of hospital performance information; and help employers provide the best healthcare benefits to their employees. The organization has focused significant research on ICUs.
[2] A Comparison of Critical Care Research Funding and the Financial Burden of Critical Illness in the United States, Critical Care Medicine 2012, Volume 40, Number 4, page 1072
[3] Critical Care, Critical Choices: The Case for Tele-ICUs in intensive Care, New England Healthcare Institute and Massachusetts Technology Collaborative, 2010, pages 5-6
[4] Leapfrog reported in May 2012 that 699 Hospitals met their ICU intensivists staffing standards. AHA reports 5724 hospitals. The resulting percentage is 12.21%.
[5] Data source: Advanced ICU Care. The company benchmarks its performance against APACHE IV mortality and treatment al algorithms.





