August 16, 2016

Being American: How Exceptionalism Is Transforming U.S. Healthcare
Midway through the Rio Olympics, the prowess of the diverse, raucous and remarkably talented U.S. team is on full display. We marvel at the athletes’ dedication. Their enthusiasm is infectious. Their athleticism is spellbinding. They represent America at its best, and all Americans can be justifiably proud.
It’s been one long samba line to the medals stand. With only 4.3% of the world’s 7.4 billion population, the U.S. has captured (through August 14th) almost 14% of the awarded medals.
The U.S. team embodies the restless, forward-moving, get-things-done mindset that fuels America’s innovation engine. Their brilliant accomplishments exemplify America’s unique ability to tackle large challenges and emerge victorious. They personify both the American dream and American exceptionalism.
The United States confronts no bigger challenge than fixing its broken healthcare system. It harms too many people and consumes too much national wealth. As we revel in our Olympic team’s success, it’s worth considering how American exceptionalism continuously shapes and transforms our national existence.
This is as it should be. American exceptionalism created the country’s current bloated and inefficient healthcare system. Only American exceptionalism can fix it.
Values Proposition
It is impossible to understand U.S. healthcare without understanding how deeply American exceptionalism is woven into U.S. identity and culture. To an extent, this is a truism. Any enterprise so expansive that it consumes 18 percent of GNP, employs millions and touches all citizens will reflect national identity and values.
Moreover, the system’s size and complexity combined with its structural anomalies (the independence of physicians, the predominance of nonprofit hospitals, the variation in third-party payment) make broad generalizations about U.S. healthcare impossible. Contradictions abound.
For example, Americans support their local not-for-profit hospitals through expansive philanthropic and volunteer support. At the same time, Americans expect hospitals to maintain financial viability and raise capital in the private capital markets. Mission collides with profit-making. Hospitals struggle to navigate between these competing currents.
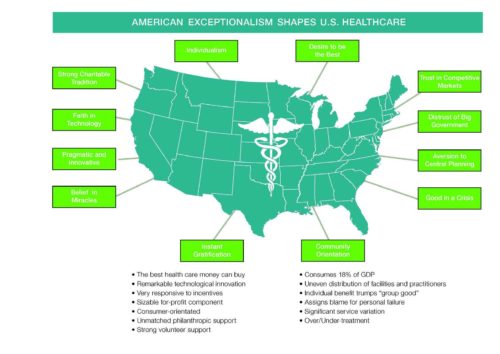
In 2008, Nancy Kane (Dean of the Harvard School of Public Health) and I wrote “The U.S. Health System: A Product of American History and Values.” centered on the values chart presented above. Our analysis examined how American values have influenced U.S. healthcare’s design and operation. Oxford Press published our white paper in 2010 as part of an anthology on fragmentation in U.S. healthcare.
The values chart arrays several quintessential American values around a U.S. map and distills their positive and negative effects in bullets below the map. The relationships between these American values are complex, interrelated and deeply held. They also complicate ongoing attempts to reform healthcare payment and service delivery.
Exploring core American values illuminates the contours of the healthcare policy debate. It is ironic that these core American values create U.S. healthcare’s contradictory and often perverse characteristics.

Exceptional American Healthcare
Once the Olympics conclude, America’s politically-divided populace will turn its full attention to a divisive presidential election with two deeply-unpopular candidates with polar-opposite positions on the Affordable Care Act. Hillary Clinton wants to improve Obamacare. Donald Trump wants to obliterate it.
During this election-charged policy debate, it is timely to revisit how American values influence American healthcare. These values reflect inherent tensions embodied in the political debate regarding access, value, transparency and government’s proper role.
Beyond political rhetoric, these core American values shape our national attitudes, dialogue and policies regarding healthcare reform. In this sense, the Democratic and Republican parties actually agree more than they disagree.
Let’s examine the following four from the values chart presented above: individualism; distrust of big government; good in a crisis; and faith in technology.
- Individualism: Individualism trumps the collective good. When it comes to healthcare, Americans want the best and want it now. Doctors and hospitals want to be the best. They demonstrate their superiority through awards and investment in cutting-edge technologies. Without normal market constraints, these behaviors fuel costly and unsustainable investment in acute care services and facilities.
Americans believe in individual responsibility. American grant credit for individual successes and assign blame for individual failures. This largely explains America’s national tolerance for coverage gaps and large numbers of uninsured citizens.
Distrust of Big Government: Revolutionary war patriot and author Thomas Paine captures the sentiment concisely in this quote, “that which governs least governs best.” Americans are uncomfortable with large, centralized government programs. Unlike over 40 other countries and despite several attempts (most notably in 1948 under Truman and 1994 under Clinton), the U.S. has never enacted national health coverage.
Americans naturally distrust “big-government” solutions. In contrast, the ACA’s core provisions (the individual mandate, state health exchanges and risk corridors for insurers) are market-based concepts originally conceived by conservative think tanks. It took a Democratic president and Congress to enact Republican-inspired comprehensive healthcare reform legislation.
- Good in a Crisis: Americans rise to the occasion. In two world wars, numerous international disputes and untold natural disasters, Americans lend their people, energy, resources and money to address big challenges.
Not surprisingly, the American healthcare system goes the extra mile in times of crisis. Americans don’t accept death naturally and go to unprecedented lengths to avoid and delay it. This translates into more surgeries, more complex drug regimens, more extensive end-of-life care and much higher per-capita treatment costs.
- Faith in Technology: America is the world’s innovator. Our awe-inspiring breakthroughs in communication, data processing, entertainment, retailing and engineering have transformed human life. We invest because we want solutions and believe we can find them.
American medicine has a remarkable history of discovery and innovation. At the same time, Americans lead unhealthy lives and expect surgical procedures and pills to solve resulting medical problems.
Americans’ energy, instincts, individualism and impatience have shaped our healthcare delivery system. In response, the system has ballooned into an acute-care-centric delivery model that is financially unsustainable.
Even more alarming, the American healthcare system fails to address the country’s most pressing health need: exploding chronic disease. Paradoxically, there is ample funding in the system to amputate a foot, but limited funding to manage the diabetes that necessitates the amputation.

Going for Gold
Economist Herbert Stein noted, “Trends that cannot continue, won’t.” One way or another, the American health system will adjust its cost structure to current funding realities. Americans confront a stark choice: either accept rationing of healthcare services or transform the system so that Americans receive greater value (better outcomes, lower costs, greater convenience) for healthcare expenditure.
It’s implausible to believe Americans will accept healthcare rationing. It’s not in our DNA to do so when American ingenuity can create business models that align payment with efficient delivery of superior healthcare services. This is already happening.
Like America’s Olympic athletes, America’s best health companies are not satisfied with incremental improvements on a flawed delivery system. They’re focused on winning. Their relentless efforts will lead to the following transformational shifts in U.S. healthcare:
- Market-Based Solutions: the Affordable Care Act has triggered an unprecedented level of investment in market-based strategies (e.g. Walmart’s movement into primary care) designed to exploit the current system’s weaknesses. Theses market-based reforms will expand, evolve and reconfigure the current delivery model to better meet customer needs.
- Normalizing Supply-Demand Market Dynamics: healthcare is shifting from an artificial marketplace where supply drives demand (i.e. the best predictor for cardiology procedures is the number of cardiologists) to a normalizing market where supply adjusts to intrinsic demand. Bundled payments for specific treatments; Medicare Advantage programs; and employers contracting directly with providers for health services are payment models that support this market shift. These types of payment approaches and aligned business models limit overtreatment, increase facility productivity and incentivize better chronic disease management.
- Rationalized Service Pricing: improved outcome measurement will reduce differential pricing for covered services. Commercial rates will migrate toward lower governmental rates. Hospitals will have less ability to cover the cost of unprofitable research, training and community education programs. Concurrently, hospitals will begin to charge patients for amenities.
- Consumerism: winning health companies will balance prevention with treatment and provide comprehensive health and wellness services. Health companies will become consumer-driven organizations that develop strong brands and deliver exceptional service. As in all consumer industries, customers will choose brands they trust that deliver value.
- Proliferating Low-Cost Technologies: activity monitors, convergence media platforms, remote sensors, avatar coaches, distance consults, self-service kiosks and bio-metric scanners are examples of scalable, low-cost technology solutions that improve care delivery. As they compete for market acceptance, these innovative technologies will disrupt current practices and adapt to customer need. Most importantly, they will improve care quality/outcomes and lower costs.
- Expanded Primary Care: lifestyle improvement, particularly chronic disease management, requires continual customer engagement. In response, providers and payers are expanding primary care service locations, relying more on non-physician caregivers, experimenting with alternative business models and aligning with social media. Better tools, accurate information, emotional support and improved living/working environments are essential for reversing unhealthy behaviors and improving community wellbeing.
Rampant Irony: “The Enemy is Us”
People around the world admire and often seek U.S. healthcare. For complex acute conditions, American healthcare is the best money can buy. Overall, however, the American healthcare system is defective. It is unwieldy, unfair and ineffective against chronic disease. It leaves too many citizens unprotected, unduly rewards vested interests and causes too much physical, emotional and financial harm to patients.
Sadly, it is easier to blame some evil other guy (bad government, greedy insurers, arrogant administrators, rich doctors) than to acknowledge that America’s fragmented healthcare system reflects strongly ingrained American beliefs, contradictions and mythology.
Failure to address the U.S. healthcare’s structural flaws weakens America’s global competitiveness, reduces its standard of living and contributes to widening socio-economic disparities. These unfortunate results represent an ironic manifestation of American exceptionalism. As the famous Pogo cartoon observes, “We have met the enemy and he is us.”

Farther, Higher, Faster, Stronger
Throughout history, Americans have responded to crisis with determination, creativity and bold action. If Pogo is right, it’s time to dig deep, acknowledge failure, learn from it and relentlessly improve service delivery. A new American healthcare system must center on “tried and true” market principles that reward value creation.
It’s not enough for American healthcare to become as good as that provided in other advanced economies. With breakthrough business innovation, American healthcare can leapfrog their centralized healthcare systems with better resource allocation, more innovative solutions and greater customer engagement.
As in the Olympics, results are what counts in healthcare: better outcomes; lower costs; greater convenience; healthier communities. Multitudes of athletes aspire for Olympic glory, but only a select few experience it. The rest of us live vicariously.
For consumers, accessing decent, affordable healthcare should not require an Olympian effort. It will and should be an Olympian endeavor for health companies to earn customers’ trust by consistently delivering superior and tailored healthcare services. Winning health companies will demonstrate every day that outcomes matter, customers count and value rules.





