December 12, 2018

Frontline Decisions in Real Time: What Health Systems Can Learn from the U.S. Military’s Defeat of Al Qaeda in Iraq
 “The teams were operating independently—like workers in an efficient factory—while trying to keep pace with an interdependent environment. We all knew intuitively that intelligence gathered on AQI’s [Al Qaeda in Iraq] communications and operations would almost certainly impact what our operators saw on the battlefield, and that battlefield details would almost certainly represent valuable context for intel analysis, but those elements of our organization were not communicating with each other.”
“The teams were operating independently—like workers in an efficient factory—while trying to keep pace with an interdependent environment. We all knew intuitively that intelligence gathered on AQI’s [Al Qaeda in Iraq] communications and operations would almost certainly impact what our operators saw on the battlefield, and that battlefield details would almost certainly represent valuable context for intel analysis, but those elements of our organization were not communicating with each other.”
—General Stanley McChrystal from Team of Teams
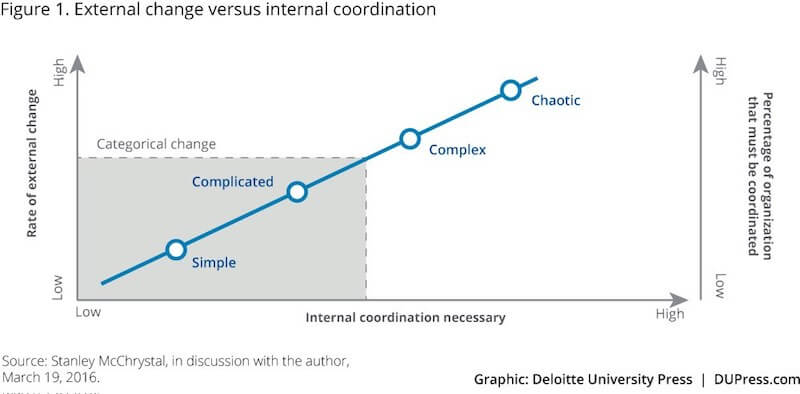
By 2004, Al Qaeda in Iraq (AQI) was routinely defeating U.S. forces on the battlefield by employing asymmetric, hit-and-run tactics that distributed command control and placed a premium on speed. Networked and non-hierarchical, AQI was a new, formidable type of enemy.
Recently appointed commander General Stanley McChrystal knew doubling down on current strategies would not reverse the tide. It was time to think differently. McChrystal created a task force to analyze how a fragmented, ill-equipped enemy was beating the world’s most-qualified and best-equipped military force. He wanted to understand why the military’s long successful hierarchical command structure was failing.
The task force determined that leaders at central command consistently made the wrong tactical decisions because they lacked real-time information and situational context. Data about AQI moved through military intelligence more slowly than the enemy moved in the field. Traditional command-centric management models focus on planning and prediction. When using this reductionist management model, the military was unable to respond effectively within an increasingly complex and unpredictable environment.
Efficient decision-making mechanics, the key feature of centralized management, had become brittle and lacked resilience. Processing data, permissions and orders to act through the chain of command delayed decision making. Delay paralyzed frontline troops, who were ready for battle but lacked information and authority to engage the enemy successfully.
The bottom line was that the battle in Iraq had become more complex and dynamic as AQI players applied interconnected technologies (e.g. mobile phones, texts, photos) to guide their battle tactics. This complexity and dynamism created continuous unpredictability for U.S. forces.
McChrystal realized that he needed a new command structure to respond effectively to the AQI threat. U.S. forces needed to organize and act with adaptability and resilience to succeed on the field of battle. His success creating a flat, adaptable, resilient command structure turned the tide in Iraq.
The same combinations of complex and dynamic operating conditions hamper the effectiveness of frontline caregivers in U.S. health systems. They lack real-time data and authority to optimize care decision making and outcomes. The military’s lessons learned in Iraq have direct applications to U.S. hospitals.
FROM THE BATTLEFIELD TO THE HOSPITAL FRONTLINE
U.S. healthcare has the best-trained clinicians, the best equipment, and the best facilities in the world, but operates inefficiently, makes too many mistakes, frustrates patients and burns out frontline personnel. This underperformance occurs despite hospitals possessing the necessary components of highly efficient and reliable organizations: digitized medical records, gigantic data warehouses, elaborate protocols and centralized performance monitoring.
Like the U.S. military in Iraq circa 2004, the U.S. healthcare system is failing, and it is failing for many of the same reasons.
Managerial architecture designed for production efficiency lacks adaptability and resilience. Centralized control reduces situation-al awareness and data flow. This results in unnecessary patient harm and excessive waste of resources.
Historical management theory is partly to blame for performance failures. The industrial age’s primary managerial goal was achieving efficiency at scale. Management systems built to optimize efficiency systematically plan for predictable actions and processes. Technology has changed operating dynamics and they’ve become more complex, but healthcare’s managerial models have yet to adapt to this new reality.
Today, we live and work in an interconnected, technology-heavy world. Healthcare technology has advanced capabilities but pulls clinicians away from patients while making care more expensive. Hospital operations are anything but linear and predictable. Just as McChrystal’s forces failed when applying traditional management models in unpredictable, complex environments, so too do hospital operations fail.
It’s time for a new way to operate. Health system leaders need to build new organizational architecture to manage the inherent complexity of hospital operations. Fortunately, the military has highly relevant examples for implementing organizational rede-sign, pressure tested on the frontlines.
BUILDING RESILIENCE AND ADAPTABILITY AMID CHAOS
In his 2015 book Team of Teams, McChrystal outlines the ways he drastically altered the strategy and operating environment of troops. His three core lessons offer a blueprint for healthcare leaders to take action.
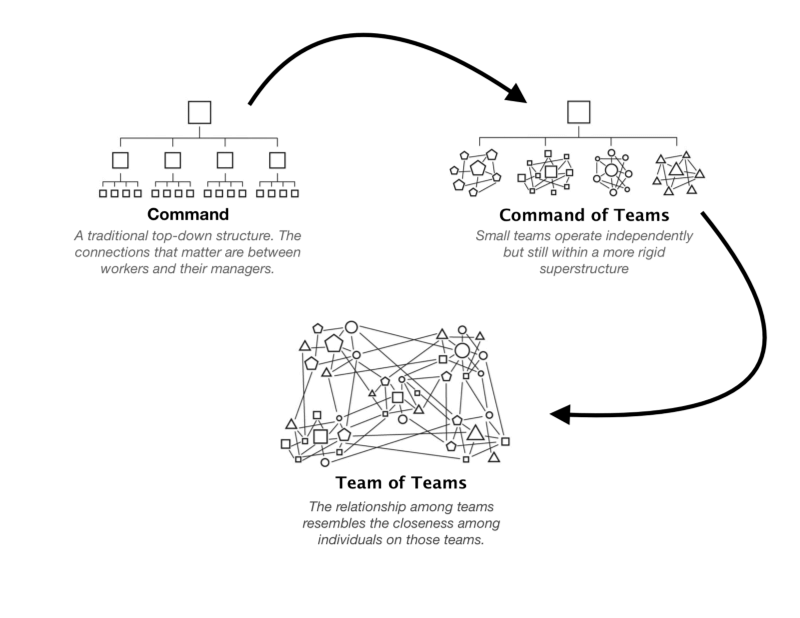
Lesson #1: Shift from a “Command of Teams” to a “Team of Teams” Model.
McChrystal realized AQI’s command structure was not hierarchical. It consisted of a dispersed network of connected groups that shared a common purpose and exchanged extensive information. In contrast, U.S. Forces used a central command center to control operations. The high quantity and velocity of information overwhelmed central command and limited its ability to guide frontline personnel. (1)
The U.S. Armed Forces organization had numerous teams, but they operated in silos under a rigid command superstructure. McChrystal characterized this as the “Command of Teams” structure. While the individual teams could adapt when operating independently, they lacked the ability to coordinate their efforts to achieve organizational goals. McChrystal needed to replicate the effective traits of small teams (trust, situational awareness, common purpose, shared information) at scale.
McChrystal’s solution was to create a “Team of Teams,” an organizing model where the operating dynamics of effective teams replicate themselves throughout the entire organization. Teams that previously operated in silos came together as one with a single “shared consciousness.” In essence, he created a network to defeat a network.
Across health systems today, formal and informal teams must navigate through increasingly complex operating environments to make effective decisions in real time. Current management systems fail to develop the trust and information sharing required for teams to solve dynamic problems in real time. Frontline caregivers undertake heroic actions to overcome legacy systems so patients get the services they require.
Healthcare’s teams of teams cannot function until organizational architecture equips them with the information they require and the authority to use it in real time.
Lesson #2: Arm teams closest to the problem with decision-critical, system-level information.
McChrystal realized that frontline teams needed faster access to information to make the right operational decisions. Task Force members needed to operate within an interconnected and decentralized system, not through a central command structure. Information had to be transparent and available to all members.
McChrystal’s team assembled the Situational Awareness Room, a vaulted, heavily fortified chamber with large computer screens. But it wasn’t the technology alone that unlocked collaboration between his teams, it was what the technology enabled his teams to practice.
The Situational Awareness room supported information-sharing techniques proven to drive collaboration and performance. These included the following: 1) face-to-face interaction; 2) direct, peer-to-peer communication between teams, not channeled through a leader; and 3) opportunities for side conversations.
With this new communications system, McChrystal’s teams could share the right amount of data and contextual information with each other in order to act in real time. McChrystal convened a 90-minute daily video conference at 9 a.m. to share vital information with all task force members, eventually 7,500 people throughout the globe.
Despite deep investments in technology, training, and improvement initiatives, health systems struggle to get real-time information to the decision makers on the frontline who need it to act. Decision-critical data is often stored layers deep in centralized systems (such as EMRs), and it’s not translated into an easily digestible form. Sometimes it’s not even collected. Most data is historical, not real time, which leads to retrospective analysis rather than present action.
Additionally, health systems with traditional command centers mostly centralize information into the hands of key decision makers. Just as McChrystal realized, these central command structures often fail to respond to real-time events. Instead, health systems need capabilities to relay real-time information to empower the frontline to collaborate to their full potential, as highly adaptive and reliable teams.
Lesson #3: Build trusted relationships among traditionally siloed teams. While shared information forms a common understanding of objectives between teams, McChrystal needed to create strong relationships between teams to solve system-level issues. Teams needed to understand how others made decisions. With a shared thought process and trust, teams could act independently with a sense of the whole mission, and make individual decisions that advanced the overall mission, not just their component.
McChrystal took a low-tech approach to building relationships and trust. He cross-fertilized teams and established liaison programs. Over time, the trust between individuals grew into trust between teams that, when paired with the common purpose, fostered unprecedented levels of cooperation.
For health systems desiring adaptive managerial architecture, real-time information and technology are not enough Relation-ships matter and trust is the glue that binds teams together. For frontline staff to take system-level actions based on real-time information, they need to trust teams in other departments and facilities are acting to achieve optimal system-wide performance, not individual-unit performance.
ACHIEVING A “TEAM OF TEAMS” MODEL IN HEALTHCARE THROUGH TECHNOLOGY
Today, examples of forward-thinking health systems adopting this team-of-teams approach are emerging. These health systems seek to build more resilient, adaptive organizations to achieve better outcomes and improve margins.
One example is Fairview Health Services, a health system that operates 12 hospitals and medical centers and 9 emergency departments in Minnesota. Like the best performing teams, it has well-trained, well-intentioned people and well-equipped facilities.
 Fairview determined the team-of-teams management model would be the best approach to deliver a more consumer-centric experience for its patients.
Fairview determined the team-of-teams management model would be the best approach to deliver a more consumer-centric experience for its patients.
Leadership knew however, that a team-of-teams model wasn’t possible without a new technology and communication platform that could harness the operational data necessary for real-time actions. Without a real-time communications platform, Fairview’s frontline teams would default to finding and interpreting retrospective data from multiple sources to guide their moment-to-moment decisions. This approach generates subpar outcomes and adds unnecessary stress.
 To implement this team-of-teams management model, Fairview partnered with Qventus, an artificial intelligence-powered solution that optimizes patient flow. The Qventus platform ingests data from Fairview’s EHR and other systems. It then provides real-time operational and clinical data to frontline personnel who coordinate care within and between Fairview facilities.
To implement this team-of-teams management model, Fairview partnered with Qventus, an artificial intelligence-powered solution that optimizes patient flow. The Qventus platform ingests data from Fairview’s EHR and other systems. It then provides real-time operational and clinical data to frontline personnel who coordinate care within and between Fairview facilities.
With this system, Fairview’s frontline teams can see the larger picture, predict events from real-time data, and make course corrections in real time. The system pushes the necessary data to the frontline at the moment it’s needed to provide a “nudge” of the optimal action.
Fairview uses a combination of its existing protocols and intelligent interventions from Qventus to identify operational barriers in real time and coordinate the cross-functional collaboration required to streamline patient placement, discharge planning and address ED surges. 
Fairview CEO James Hereford describes the essentiality of liberated data flow to organization’s larger purpose as follows,
“I see this as one of the critical capabilities necessary to transform the experience of our patients, and it is part of a larger strategy to redefine how a care delivery system works.” —James Hereford, Fairview Health CEO
TOWARD THE TEAM OF TEAMS VISION
Just as the team-of-teams management model and infrastructure helped U.S. forces in Iraq outmaneuver AQI, health systems can use this model to help frontline teams assess and solve problems in real time on their own authority, within the context of overall mission goals.
Systems like Qventus help hospitals operationalize the team- of-teams approach, providing frontline teams with the data, tools, trust, and authority to act constructively on behalf of individual patients and the overall organization. Managers and charge nurses get patients into beds with less friction. Discharges occur seamlessly. ER diversion disappears.
These systems proactively identify bottlenecks where patients and providers wait for direction. They minimize error. They em-power frontline staff. They optimize operational flow by balancing people, equipment and facilities at capacity. Through this technology, hospital executives can see new ways tp make their asset-heavy systems more efficient and increase margins.
Most importantly, rethinking technology, communication and management models improves patient outcomes and satisfaction while reducing provider burnout. Ultimately it creates reliable hospital operations that pay dividends in better patient care, better patient experience, better outcomes, and better margins.
Outcomes Matter. Customers Count. Value Rules.
SOURCES
- https://www2.deloitte.com/insights/us/en/deloitte-review/issue-19/general-stanley-mcchrystal-interview-innovation-in-leadership.html
- https://medium.com/@beaugordon/key-takeaways-from-team-of-teams-by-general-stanley-mcchrystal-eac0b37520b9
CO-AUTHOR
 Mudit Garg serves as the CEO and Co-Founder of Qventus. Qventus’ AI-based platform is the first “System of Action” that brings together data, technology and people to make it possible for hospitals to run their operations efficiently, in real time and at scale. In his role at Qventus, Mudit works with more than 70 of the top health systems across the country, including academic, community and safety net hospitals. Mudit was recognized for leadership as one of the Silicon Valley Business Journal’s 40 Under 40 and as one of the Top 30 Healthcare Leaders Under 40 by Business Insider. He earned his Master’s in Business Administration and Electrical Engineering from Stanford University and also holds a Bachelors from the Indian Institute of Technology.
Mudit Garg serves as the CEO and Co-Founder of Qventus. Qventus’ AI-based platform is the first “System of Action” that brings together data, technology and people to make it possible for hospitals to run their operations efficiently, in real time and at scale. In his role at Qventus, Mudit works with more than 70 of the top health systems across the country, including academic, community and safety net hospitals. Mudit was recognized for leadership as one of the Silicon Valley Business Journal’s 40 Under 40 and as one of the Top 30 Healthcare Leaders Under 40 by Business Insider. He earned his Master’s in Business Administration and Electrical Engineering from Stanford University and also holds a Bachelors from the Indian Institute of Technology.




