April 21, 2020
Health Tech to the Rescue: Combatting COVID-19 with Virtual Care and Predictive Analytics
With stunning swiftness, COVID-19 knocked America’s healthcare delivery system to its knees.
A month into the crisis, normal hospital operations are in upheaval. Avoiding in-person care has become the norm and the volume of admissions, surgeries and ER visits has plummeted. Overwhelming demand for ICUs, ventilators and personal protective equipment (PPE) has strained delivery and supply chains to the breaking point.
The human drama has been tragic, heroic and heartwarming. Separated from loved ones, many patients are dying alone. In regions where spread is rampant, frontline clinicians work nonstop at risk of their own lives. To show their gratitude, New York City’s locked-in residents applaud, whoop and bang pots and pans outside their windows every evening at seven.
America’s fragmented, uncoordinated healthcare system has proven to be highly vulnerable to the fast-spreading contagion. The impediments to sharing data and information between systems and across regions are more frustrating and lethal than ever. Government and public health leaders are struggling to determine the availability of critical resources, and face systemic
obstacles to allocating needed resources effectively.
In response to this new COVID-19 reality, healthcare is reconfiguring itself in real time.
Most providers are using virtual care platforms to treat patients. Government agencies have eased regulatory restrictions to expand virtual care access and delivery. Public health officials and researchers are also using big data and analytics to identify hotspots, track disease spread, predict severity and allocate resources.
In a fascinating twist, health IT startups are meeting these expanded service demands with proven but underutilized tech-based solutions that scale quickly and massively.
Unlike more innovation-friendly industries, healthcare IT companies have struggle mightily, often for years, to overcome cultural, regulatory, reimbursement and workforce barriers to adoption. COVID-19 has swept those barriers away. Health IT is bridging gaps in a system under siege.
Elastic Demand for Virtual Care
Healthcare organizations of all types are using virtual care solutions to to increase access to care providers, limit disease spread and engage patients. Today, nearly 300 U.S. vendors offer virtual care services. They range from patient-doctor video links to sophisticated platforms that incorporate AI, chatbots and other advanced technologies.
The government is helping. CMS implemented emergency changes to telemedicine licensure[1] and reimbursement laws[2] to facilitate telemedicine adoption in response to COVID-19. Providers have quickly encountered a new problem, however: the volume of demand is straining capacity.[3]
The nation’s largest independent telemedicine provider, Teladoc, experienced a 50% increase in demand for its services through March 20, 2020. As a result, patients are reporting lengthy wait times even as Teladoc adds more physicians.
This is a predictable outcome. As happens with many new technologies, traditional telemedicine replicates rather than leapfrogs existing process. Most telemedicine visits are virtual versions of face-to-face clinic visits with waiting rooms, real-time video conferencing/data entry, and follow-on prescriptions.
In contrast, Minneapolis-based Zipnosis offers an innovative, sequential approach for health systems. It is low cost, highly efficient and scalable.
Launched 10 years ago by CEO Jon Pearce, Zipnosis is a SaaS provider of white-label telemedicine software. Health system clients use Zipnosis as their virtual gateway for care delivery. As Pearce notes, “We started Zipnosis because we knew traditional telemedicine didn’t have the ability to truly scale.”
The Zipnosis platform automates triage, guiding patients to the most appropriate level of care based on their symptoms. A select number of conditions necessitate direct clinical attention via video, telephone or in-person. Roughly ninety percent of patients, however, receive care through asynchronous visits.
An asynchronous visit means that a patient, on his or her own time, answers a series of sequential interview questions. The Zipnosis platform transmits to providers who review patient answers on their own time. The providers then contact patients through the most appropriate channel to provide diagnosis and a treatment plan.
While real-time “synchronous” telemedicine visits take 18 minutes of clinical work time, a Zipnosis asynchronis visit averages just 89 seconds.[4] This has enabled health system customers to
meet the surge in demand for virtual care. For example, a single physician using the Zipnosis platform in Seattle, WA, diagnosed 1,077 patients in a week (12 patients per hour for 12 hours per day for 7 days).
In addition to managing elastic demand, the Zipnosis platform adds new practitioners with ease. In the midst of the COVID-19 crisis, one health system client trained 600 new clinicians to use the Zipnosis technology within three weeks through YouTube videos.
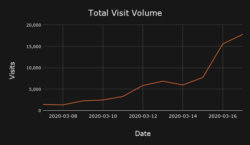
The volume of patient visits handled by the Zipnosis technology has been breathtaking.
Zipnosis experienced a 3,600% increase in utilization across its platform in the first 11 days of the COVID-19 crisis. In March, Zipnosis logged 412,553 total visits, with daily volume surging as high as 36,000. 88.2% of those visits were asynchronous adaptive interviews, 3.4% text chat, 4.5% phone calls and 3.9% in-person video. Zipnosis was the highest capacity telemedicine provider in the country during March 2020, serving four times as many patients as Teladoc Health.
Zipnosis is helping to maximize clinician and health system capacity, minimize in-person contact, capture longitudinal data, and steer the most symptomatic or vulnerable patients to nearby labs for testing. Pearce observes,
“When people say they don’t have enough doctors at a national level, that’s simply not true. What they need are more efficient processes. We’ve now proven the power asynchronous visits have in handling astronomical patient volumes.”
Better Data, Better Predictions, Better Resource Allocation
When the COVID-19 crisis hit, the CDC released guidance for assessing exposure risk. Zipnosis immediately updated its automated triage process with 11 questions that screen for COVID-19.
Currently, 33 of Zipnosis’ 51 health system clients are screening for COVID-19 and 21 are offering free COVID-19 virtual visits. Following CDC guidelines, Zipnosis conducts as many as 21,000 daily COVID-19 screenings. Their asynchronous screening process takes 4 minutes.
The Zipnosis platform categorizes patients completing the 11 COVID-related questions into five risk groups. Of the 192,915 patients screened in March:
- 14% were asymptomatic/low risk with no need for an in-person visit or test.
- 7.5% were asymptomatic/high risk.
- 4.3% were asymptomatic but had exposure risk.
- 7.5% had a cough only.
- 66.6% were symptomatic.
This is valuable information not just for patients and care providers but also for policy makers combatting COVID-19. With the right analytics and tools, such data creates insights that can save lives and resources.
Carrot Health, another Minneapolis-based health IT company, applies structured data and predictive analytics to assess COVID-19 exposure risk at the county level, nationwide.
Founded 6 years ago, Carrot Health uses robust consumer and demographic data to develop health profiles for nearly every American adult (262 million people). Carrot’s payer and provider
customers rely on those profiles and data-driven models to select more appropriate interventions, improve health outcomes, reduce care costs, design better products and enhance engagement and marketing.
As COVID-19 appeared in the U.S., Carrot Health recognized that accurate data would be critical in predicting the disease’s spread and impact. Carrot analyzed its own dataset in relation to
accumulating COVID-19 disease data from China and other countries to identify the individuals and communities most vulnerable to critical infection.
Using this information and following CDC guidelines, Carrot applied the risk factors most associated with the disease spread and severity to assess relative risk from exposure. These included: age, gender, smoking, and the presence of diabetes, hypertension and COPD. Carrot then produced and published a predictive risk dashboard to identify which U.S. counties are most vulnerable to the COVID-19 contagion.
Visit this link to view the dashboard.
The dashboard’s purpose is not to predict disease outbreak or transmission per se, but to assess the criticality risk for individuals who contract the illness. In this way, Carrot can help identify which counties will be hardest hit and which individuals are at greatest risk for needing ICU care.
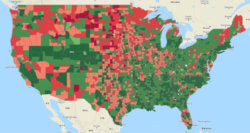
The chart provides a visual representation of Carrot’s COVID-19 risk assessment. The counties in red have the highest risk of severe impact.
Carrot’s analysis reveals that many counties are ill-prepared to handle projected infection rates, including St. Louis county in northern Minnesota with 170,000 adults. A 10% infection rate in St. Louis County translates into 17,000 COVID-19 cases with 1,820 requiring ICU care. Since the county only has 78 ICU beds, it must adopt active measures to prepare to treat critical COVID-19 patients.
Carrot’s predictive risk models are Bayesian in nature, meaning that models improve as more outcomes data becomes available. Carrot regularly updates its COVID-19 risk predictor as more case data compiles and clinicians increase their understanding of the disease’s underlying risk factors. This is where Zipnosis comes back into the picture.
Carrot has partnered with Zipnosis to incorporate Zipnosis COVID-19 data collected through its virtual care platform. This Zipnosis data improves the weights Carrot applies to its COVID-19 risk factors, enhancing the accuracy of its predictive models and analytics.
Virtual screening and predictive analytics are helping to assess the risk and severity of infection for hundreds of thousands of people. This enables providers, testers and local governments to be more efficient and effective in allocating resources to improve treatment outcomes and slow disease spread.
As Carrot CEO Kurt Waltenbaugh notes:
“Currently, Carrot’s risk predictor modeling focuses on criticality and the potential need for ICU care and ventilators. New data sets from Zipnosis and other sources will help Carrot understand where testing is taking place, where new outbreaks are likely, and how resources can be directed most effectively.”
Zipnosis and Carrot are not alone. Other healthcare technology companies are contributing important solutions and data to improve disease spread prediction, assessment and treatment. For example:
- Durham, NC-based Validic[5], a virtual health and remote monitoring company, has developed a real-time monitoring solution leveraging wearables to observe, analyze, and triage individuals remotely for the emergence of COVID-19 symptoms. Metrics include body temperature, oxygen saturation, difficulty breathing and coughing.
- San Francisco, CA-based Kinsa[6] developed a smart thermometer to track the spread of flu in real time and forecast outbreaks 3-4 weeks in advance. Kinsa’s geographic signals are available to public health agencies, health organizations, health and wellness brands to help stop flu spread. This data helps illuminate and potentially predict COVID-19 disease spread.
- Charlotte, NC-based PeraHealth (The Rothman Index) recently introduced a tool that allows health systems to identify dischargeable COVID-19 patients. Their clinically-validated discharge filter improves hospital throughput and ICU utilization, detects deterioration in patient condition and reduces length of stay.
- Apple and Google announced jointly a system for tracking the spread of the coronavirus on iPhone and Android devices.[7]
- Amazon has created a massive public COVID-19 data set that captures and centralizes disease-specific information from multiple sources.[8]
- HCA and Google Cloud introduced the COVID-19 National Response Portal, an open data platform that promotes data-sharing about COVID-19 and its spread. It helps hospitals and communities prepare and respond to the disease.[9]
Balancing societal health with individual privacy is an acute challenge during pandemics. Some nations, including Singapore, Taiwan and Israel, are using cell phone data, wrist monitors, facial recognition cameras that monitor temperature and even drones to track the spread of infection and control movement. The best tech solutions promote health whilepreserving privacy.
Conclusion: American Healthcare at a Crossroads
America has not experienced a pandemic since 1918 and wasn’t ready for COVID-19. Better data and data sharing would have enhance national responsiveness. Given the hard-earned lessons that COVID-19 has taught policymakers, U.S. healthcare clearly needs the following:
- A national commitment to data and information sharing
- A significant shift in care delivery toward virtual solutions
- Better monitoring using IoT and big data
- A permanent loosening of unduly restrictive medical regulations
As Carrot CEO Kurt Waltenbaugh observes, “Data can dramatically enhance decision making in real time, allowing us to apply AI routines and other predictive tools to look for trends and patterns that address or prevent outbreaks.”
Yet, access to healthcare data remains a barrier to progress within U.S. healthcare. The nation lacks a national, centralized repository for all electronic medical data, and there are significant barriers to sharing even de-identified claims data.
Jon Pearce agrees with Waltenbaugh, “I think that COVID-19 exposes the weak underbelly of our claims-based data reporting system. We should have a national API with a data clearing house into which every digital health company, health plan, and provider has an obligation to share real-time data.”
COVID-19 first came to the attention of public health officials, researchers and healthcare leaders in early January. Imagine if a real-time national dataset had been available to provide actionable information to government and industry decision makers. Better data leads to timely interventions, less disease spread, less societal disruption and fewer deaths.
Treating basic patient data as a utility would enable innovative companies to develop applications that improve responsiveness, assessment and treatment. Likewise, virtual care delivered through telemedicine, automated triage and remote monitoring makes our healthcare system safer, cheaper, more accessible and convenient and less administratively burdensome.
In the 1950s, Northcote Parkinson, a British naval historian and management theorist, famously observed, “A luxury, once tasted, becomes a necessity.” Today, telemedicine and data analytics are not luxuries but crucial tools in the life-and-death struggle against COVID-19. They have introduced clinicians, patients and administrators to new levels of access, convenience, speed, efficiency, safety, engagement and data-based insights.
These luxuries, now tasted, will become necessities even after COVID-19. Virtual care and predictive analytics are essential components of a healthcare system that serves patients first. American healthcare will never be the same.
Sources
- https://www.wheel.com/blog/up-to-date-emergency-licensing-for-clinicians-1/
- https://www.cms.gov/newsroom/fact-sheets/medicare-telemedicine-health-care-provider-fact-sheet
- https://www.wsj.com/articles/telemedicine-once-a-hard-sell-cant-keep-up-with-demand-11585734425\
- Based on 2019 visit averages
- https://validic.com/blog/
- www.kinsahealth.co
- https://www.washingtonpost.com/technology/2020/04/10/apple-google-tracking-coronavirus/
- https://siliconangle.com/2020/04/08/aws-making-massive-dataset-available-coronavirus-researchers/
- https://www.modernhealthcare.com/information-technology/hca-healthcare-opens-up-covid-19-data-portal-googles-cloud
Co-author:
 Jill Frew, Managing Director Cain Brothers, is a senior banker focused on Healthcare Information Technology and Digital Health practices. Ms. Frew joined Cain Brothers in 2006 and has over 20 years of experience advising both public and private companies in a variety of M&A, capital raising, and strategic advisory transactions. Ms. Frew has executed transactions across several verticals over her career, including payer services, managed care, providers, and HCIT. Ms. Frew is a member of the Firm’s President’s Advisory Council.
Jill Frew, Managing Director Cain Brothers, is a senior banker focused on Healthcare Information Technology and Digital Health practices. Ms. Frew joined Cain Brothers in 2006 and has over 20 years of experience advising both public and private companies in a variety of M&A, capital raising, and strategic advisory transactions. Ms. Frew has executed transactions across several verticals over her career, including payer services, managed care, providers, and HCIT. Ms. Frew is a member of the Firm’s President’s Advisory Council.
Ms. Frew began her investment banking career at Wachovia Corporation as an Analyst in the M&A Group. She then worked at Wheat First Securities, focusing on public offerings and M&A advisory work for clients, primarily in the healthcare industry. Ms. Frew then spent three years as head of the Corporate Development group of PhyAmerica, where she led the M&A activity for this $1 billion healthcare services. In 1995, Ms. Frew co-founded Townsend Frew & Co., a healthcare-focused M&A boutique based in Charlotte that was later acquired by Edgeview Partners. Ms. Frew earned a BS in Finance from Utah State University and an MBA from The College of William & Mary.




