November 7, 2023

Circumcising Physician Training
The Case For Surgical Mechanics
American healthcare reputedly confronts a monumental physician shortage. A highly publicized 2021 report by the Association of American Medical Colleges (AAMC) forecasts that shortage to be as high as 180,000 physicians by 2034. [1] That’s out of a total population of roughly one million physicians.
A breathless commentary on the AAMC report by the American Medical Association (AMA) called for immediate action to forestall the crisis. [2] The AMA, like most incumbent healthcare organizations, does a good job of “admiring” the industry’s problems and offering solutions that double down on existing business practices. In Steve Jobs’ vernacular, they certainly don’t think “different.”
Regarding physician shortages, the AMA wants more funding for Graduate Medical Education (GME) funding, more residency slots, greater use of technology for expanding physicians’ reach and more investment in physician-led, team-based care. No surprises here. Physicians are still captains of the ship within a hierarchical care delivery system.
The AMA’s “solutions” are based more on preserving the status quo than on finding ways to deliver better outcomes at lower costs with great customer service. Focusing on outcomes —what disruptive innovation guru Clay Christensen described as “jobs to be done” — liberates the mind. Innovative solutions emerge that challenge conventional wisdom and practices.
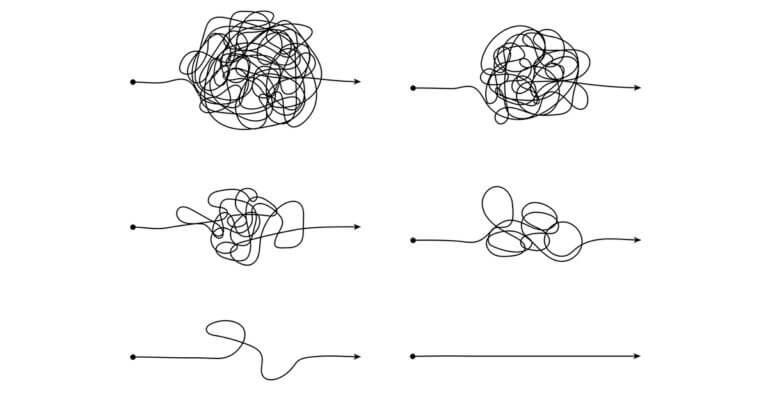
No aspect of healthcare requires “disruptive thinking” more than surgical care. It typically takes 13 years or more of training to become a surgeon of any type in the United States: four years of college; four years of medical school, three years of residency and two-plus years of a fellowship. Talk about overkill. This is the equivalent of training bicycle mechanics with the same degree of intensity as jet engine mechanics. There’s got to be a better way.
It’s Not All Brain Surgery
Not all surgeries are equally difficult to perform. Shouldn’t we train those performing surgeries to the specific mechanics of the surgeries they deliver? This thought occurred to me as I spent time recently sawing bones, threading catheters and performing internal suturing (with the help of a da Vinci robot) at the Mayo Clinic’s simulation laboratory.
Dennis Dahlen, Healthcare Financial Management Association’s current board chair and CFO of Mayo Clinic, hosted the organization’s annual strategy retreat in August at Mayo’s Rochester campus. From its origins, Mayo has believed that surgeons should not train on people. From farm animals in yesteryear to advanced simulation centers today, Mayo’s surgeons log hundreds of hours perfecting their craft.
As I progressed through the simulations, the routine and mechanical character of each surgical process was obvious. At each station, I asked why these procedures required physicians to perform them. The answer was always the same, “to intervene in case something goes wrong.”
Yet almost nothing ever goes wrong with procedures like angioplasties. These types of high-volume procedures lend themselves to focused factory operations with standby capacity for physician intervention. Medicine already does this when anesthesiologists oversee multiple nurse anesthetists.
Remote ICU monitoring/oversight is another example of allocating a scarce and expensive resource (intensivist physicians) more effectively (better care outcomes) and efficiently (lower costs). Why not expand this type of supervised care delivery to routine procedures like angioplasties?
After all, individuals who operate drones don’t need to know how to fly planes. Usually, they only have to be good at video games. Imagine how much easier and less costly it would be to find and train surgical mechanics with the narrow range of skills necessary to perform procedures skillfully.
Embracing Surgical Heresy
Logically, skilled “surgical mechanics” wouldn’t even need to attend college, much less medical school, to become adept at performing routine, high-volume procedures. This idea is heresy within medicine. Instead of using surgical mechanics where appropriate, medicine selects highly talented young people to become physicians, puts them through an excruciating training process, loads them up with debt and pays many of them high salaries to become, drumroll please, surgical mechanics. Other than to limit the supply of proceduralists and inflate their compensation, does that make any sense?
Surgical Tales
All writers love good stories. Here are three that support the concept of non-physician surgeons.
- Indian Medicine. Naresh Trehan is among the world’s most renowned cardiothoracic surgeons. Ambidextrous, he is unmatched in his skill at tying surgical knots. Trehan was the first surgeon in Asia to operate with da Vinci robots.Naresh performs as many as 30 cardiac bypass operations within a single day. He moves between operating suites to perform the critical bypass procedures. Other surgeons perform the less critical components of the surgeries. Naresh likes to joke that a “trained monkey” could replace him in the operating room.
- Snip-Snip. Sew-Sew. Mozambique has among the world’s highest incidence of HIV. Male circumcision can reduce the spread of HIV by 60%. [3] Zeke Emanuel, M.D., visited Mozambique in 2010 to witness a very successful and voluntary circumcision program aimed at the country’s young male population (ages 13-21).At a treatment center, young men waited in multiple lines to undergo the 20-minute procedure. Emanuel asked where the center recruited medical professionals to perform the procedures. The answer was both shocking and compelling: seamstresses. Already adept at cutting and sewing, the seamstresses received two weeks of training before undertaking circumcisions in the field.
- Dr. HODAD. In his book, “Unaccountable,” Marty Makary, MD, relates how residents at the Boston hospital where he trained called a popular surgeon Dr. HODAD. That nickname stood for “Hands Of Death And Destruction.” Ouch!Despite Ivy League training and an incredible bedside manner (“patients worshipped him”), Dr. HODAD was an inept surgeon who often maimed his patients. Obviously, extensive medical training doesn’t always instill the magical hand-eye coordination required to be a great surgeon or surgical mechanic.
Don’t Ask Why. Ask Why Not.
There is not a shortage of surgeons in American healthcare. There is, however, a remarkable shortage of imagination. America still trains physicians in largely the same way it did a century ago when the Johns Hopkins medical education model was proliferating throughout the nation.
Healthcare’s presumed staffing shortages create an opportunity for system redesign and innovation centered on desired outcomes, not pre-established protocols. Necessity can and should be the mother of invention. Why not lower costs and improve outcomes?
In “Back to Mathuselah,” British playwriter George Bernard Shaw has the serpent in the Garden of Eden speak these words to Eve, “You see things and you say ‘Why?’ but I dream things that never were; and I say, ‘Why not?’” Bobby Kennedy liked this phrasing so much that he adopted a similar phrase as the theme for his 1968 presidential campaign.
With regard to perceived physician shortages, we shouldn’t be asking, “Why.” With regard to imagining the creation of credentialed surgical mechanics, we should be insisting, “Why not!”
—This article originally appeared in HFMA.
Sources
- AAMC, The complexities of physician supply and demand: Projections from 2019 to 2034, June 2021.
- Robeznieks, A., “Doctor shortages are here — and they’ll get worse if we don’t act fast,” AMA, April 13, 2022.
- Prodger, J.L., and Kaul, R., “The biology of how circumcision reduces HIV susceptibility: broader implications for the prevention field,” BMC, Sept. 12, 2017.