February 18, 2025

Medical Errors Kill. Being Transparent Will Save Lives.
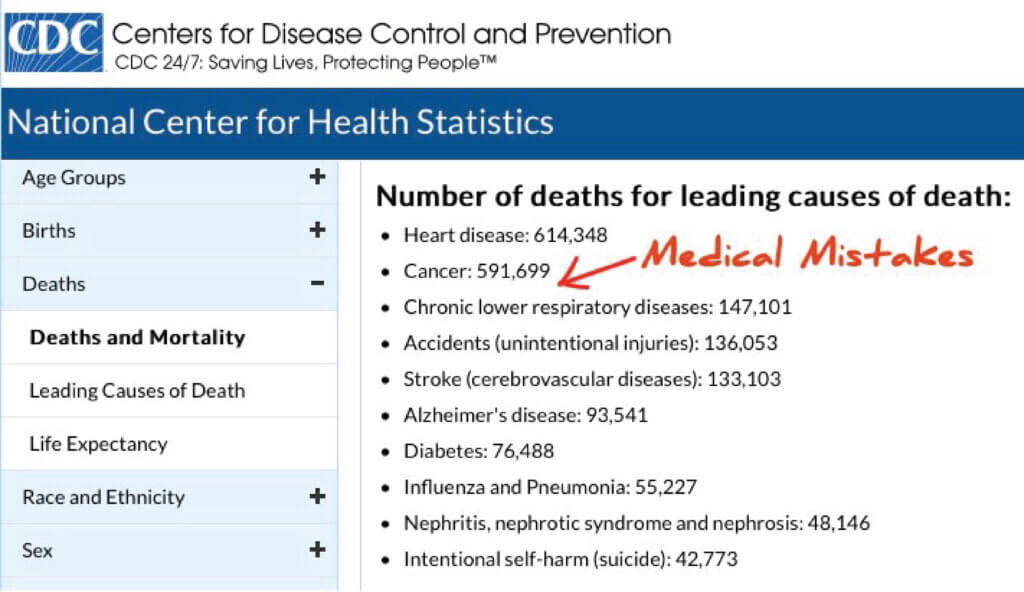
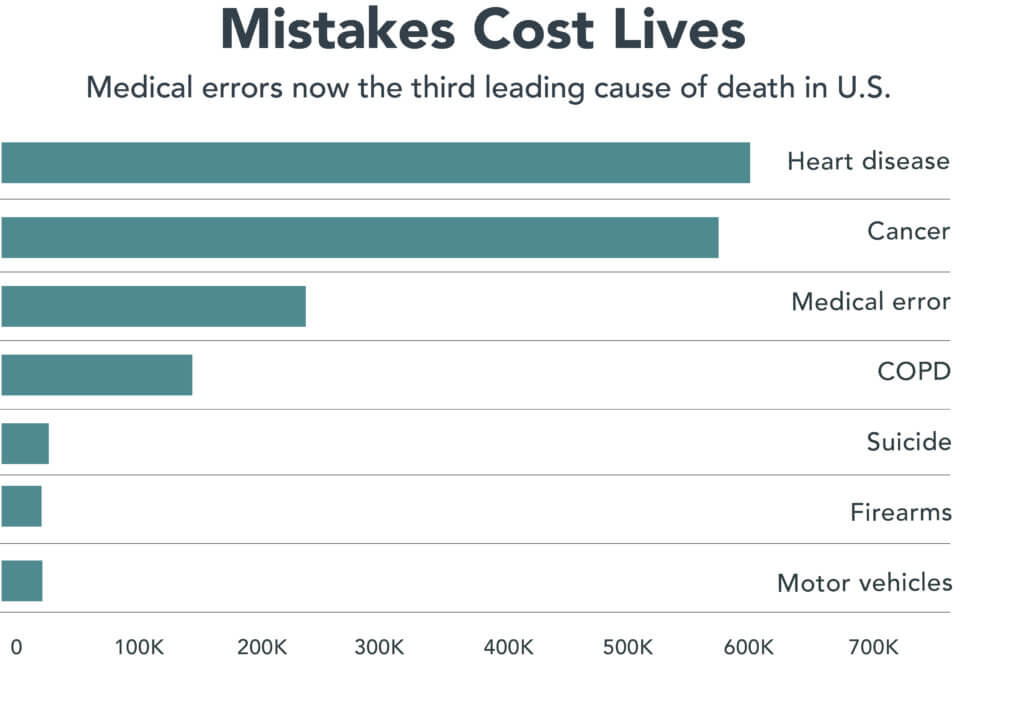
Medical injuries are the third leading cause of death in the United States. The importance of this underrecognized and upsetting fact receives little attention in the lay literature. Typically, medical injuries are combined with accidents and labeled “unintentional injuries.” Thus, heart disease and cancer, as first and second respectively, take our focus away from the third most common, noxious and avoidable cause of harm and death.
“One study reported that approximately 400,000 hospitalized patients experience preventable harm each year, while another estimated that less than 200,000 patient deaths annually were due to preventable medical errors. Moreover, the reported cost of medical errors is wide-ranging, with some experts estimating $20 billion each year and others approximating healthcare costs of $35.7 to $45 billion annually for hospital-acquired infections alone.” This statement was from “Medical Error Reduction and Prevention,” published February 2024. [1]
We, both as patients and/or caregivers, should be outraged. How can we as a nation interested in health and wellbeing not address this unsettling reality? Hiding the facts by not addressing a problem is never an effective strategy. Clearly what has been tried in the past has not been successful.
A necessary prerequisite for reducing medical errors is transparency. In the digital age, democratizing information has transformed other industries. In each example below, individuals and the public benefitted as the underlying industry improved.
- Expedia transformed the travel industry by sharing information previously available only to the travel agent. Instead of conversing on the phone while the travel agent tapped on a keyboard, travelers now have the same information at their fingertips to see all the options.
- Glassdoor brought transparency to the employment market by anonymously allowing current and former employees to share their opinions of a company’s management, culture and pay practices.
- Zillow changed real estate by providing value estimates, history and some visuals to people desiring to buy or sell property.
- Other industries and products share metrics. Consider Consumer Reports evaluations of autos, other tangible items and services.
Take the money now spent on medical marketing and image building to develop understandable metrics about outcomes to share openly with patients and caregivers. For example, what is the infection rate post-op for common procedures such as joint replacements or C-sections? What is the survival rate for different stages and grades of cancer? Most of these metrics are already easily available but hidden from the patient. One can find out more about an automobile than a health outcome.
Importantly, having the trusted source collecting, validating, collating and distributing the information should not be prejudiced by individual companies paying to use the information for marketing.
Time for Transparency
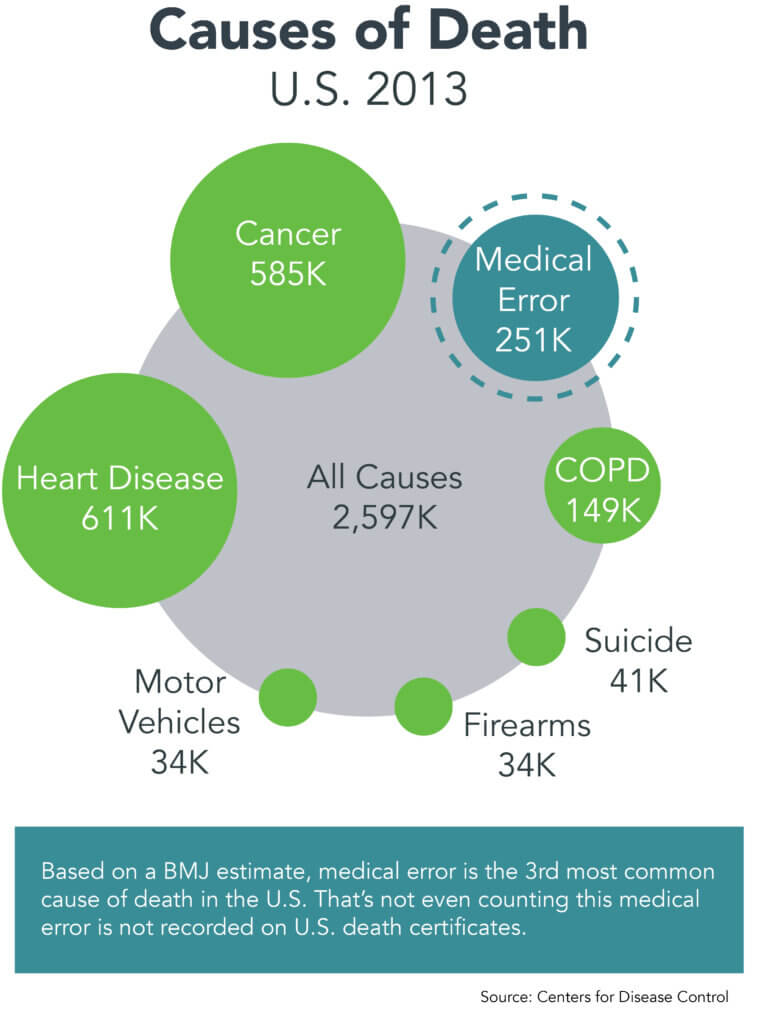 Transparency can not only save lives but also decrease costs and rally support for the healthcare industry. In addition to cost and service concerns, which are readily apparent to patients, a third more noxious but less obvious urgency exists, namely medical injuries. Costs and inconveniences are transient, but errors can maim and kill. Although medical injuries have been studied and addressed, sadly these untoward events persist. [2]
Transparency can not only save lives but also decrease costs and rally support for the healthcare industry. In addition to cost and service concerns, which are readily apparent to patients, a third more noxious but less obvious urgency exists, namely medical injuries. Costs and inconveniences are transient, but errors can maim and kill. Although medical injuries have been studied and addressed, sadly these untoward events persist. [2]
“Adverse events were identified in nearly one in four admissions and approximately one-fourth of the events were preventable. These findings underscore the importance of patient safety and the need for continuing improvement.” This conclusion published in the New England Journal of Medicine (NEJM) in January 2023 highlights the need to not only share information with potential patients but also encourage healthcare systems to emulate best practices from others, both within and out of healthcare, already benefiting from avoiding preventable mistakes. [3]
The responsible healthcare industry has been sharing best practices for decades focused on preventing harm. Unfortunately, progress has been slow. A subsequent NEJM editorial in April 2023 detailed three upsetting reasons for the lack of progress. [4]
- In 1997, a focus on “human error as a cause of accidents and adverse events,” was correctly rejected. However, the patient-safety movement remained fixated on “human error.” Improving the complex sociotechnical systems responsible for adverse events has been recognized and now accepted as the best way to decrease harm.
- Learning how to avoid illness has been under-resourced compared to the billions of dollars expended to treat self-induced disease. Starting an anti-smoking campaign with youngsters in late elementary school is very effective, costing only $300 per Quality Adjusted Life Year (QALY). QALY is a metric used by epidemiologists to describe one year of healthy living. Adding one QALY to a 70-year-old woman with tobacco-induced lung cancer costs $700,000. Clearly deterrence through education in early adolescence saves money and, more importantly, misery.
- Healthcare professionals addressing patient safety, although highly motivated, didn’t take advantage of other industries’ successful safety science expertise. Fortunately, examples from the aviation industry such as “time outs” have become standard in most healthcare procedures.
Instead of shaming altruistic caregivers, quality experts in the healthcare industry should focus on sharing outcomes. After all, who hasn’t made a mistake? Best practices can then be copied, which will benefit both the care receiver and the caregiver.
Presenting and collating information in an understandable and revealing format helps everyone — patients, families, physicians, advanced practice providers, device manufacturers, pharmaceutical firms and insurers. Digital technology has already transformed medical records and artificial intelligence is rapidly entering the healthcare industry.
What happens when a middle school child’s sub-optimal report card goes up on the refrigerator? Typically, rewards are shared, motivation improves and/or some other behavior is encouraged. The same occurs in some areas of healthcare when patients and families look for objective results.
Excellent Websites and Opportunities for More Transparency
Currently, various shades of transparency exist in healthcare. As previously shared in the January 2024 4sight Health commentary, “Your First Choice Is Your Most Important Choice,” the following makes the point specifically about transparency helping everyone — patients and caregivers. [5]
The Society for Thoracic Surgery shares specific information, down to an institution. Thus, a person requiring nonurgent cardiac bypass surgery can improve his or her odds by examining the Society for Thoracic Surgery that reports surgical outcomes by institution on Adult Cardiac Surgery, General Thoracic Surgery and Congenital Heart Surgery with grades of one to three stars. [6]
The Centers for Disease Control and Prevention’s (CDC) Assisted Reproductive Technology has information at a state level but was not easily available in the past down to an individual center until a mandate from Congress changed the playing field in favor of a couple trying to have a child. [7] Notably, in-vitro fertilization statistics have matured over the years with the CDC now supporting National Assisted Reproductive Technology. This site shares success specifics for individual centers. [8]
Interestingly, organ transplant successes broken down by institution are not yet readily available to patients, but do exists for providers. Organ transplant success statistics have been organized by the United Network for Organ Sharing (UNOS). Thus far, UNOS has focused successfully on increasing the number of successful transplants, which is noble but incomplete. The information comparing programs is known to the professionals with plans to share these facts with the public in the future. A potential recipient of an organ can improve his or her chances of survival by being informed. [9]
The lifesaving answers to the question, “Where can a patient go with the best five-year survival for a kidney, liver, lung or other organ,” should be readily available for everyone. The days of asymmetrical information are long gone. Soon AI may be able to quickly deliver the correct answer. [10]
Cancer is a special case due to its prevalence and the importance of the first choice being the most important choice. Forget about media image campaigns or your neighbor’s friend’s anecdotal experience and get the facts.
Unfortunately, cancer survival statistics are aggregated and not easily accessible to patients when they hear the dreaded words, “You have cancer.” Aggregated information is readily available from the CDC and National Cancer Institute that is no doubt important but almost irrelevant in the heat of the moment to find the optimal outcomes.
New cancer diagnoses are staged for location, size, spread locally and distantly. Patients’ functional status at the beginning of therapy can also be measured and employed to assess their ability to withstand treatments. When these two measures are combined, cancer centers’ outcomes, i.e., five-year survival, quality of life and other important metrics, can be compared one to another. Not only will patients choose cancer centers with better outcomes, but the cancer center’s desire to improve will encourage emulating other’s best practices. After a brief uncomfortable time (recall a report card with room for improvement posted on the refrigerator door) everyone’s outcomes will move in the right direction and the spread between the best and worst will narrow. [11, 12, 13, 14]
Currently, healthcare systems’ marketing on billboards, arenas, print, media and other venues typically doesn’t include survival rates or successful attainment of the desired goal, i.e., one baby not six on the first round of intro-fertilization for a couple desiring to start a family. Healthcare systems could easily focus on the Centers for Medicare and Medicaid Services (CMS) or Leapfrog, which are both objective and the foundation of many of the other marketing “bragging rights.” These later sites use subjective polls that are more akin to popularity contests rather than objective outcomes. Healthcare institutions do not pay to participate with the CMS. Really, if you have a dreadful disease, you want cure rates to decide where to get care. Expensive image marketing may or may not have any relationship to reality.
Conclusion
Transparency focused on quality outcomes is an attribute that both helps health systems and potentially cures patients. All patients or caregivers should know true quality of the care metrics. Other industries such as travel, employment and real estate, for example, have been transformed for the better. With digital records, computerization and everyone’s desire to decrease medical errors and improve outcomes, the opportunity to improve is right before us. Let’s improve both the caregivers’ and care receivers’ lives, which will help restore the faith and trust the public wants to have with the healthcare industry.
Sources
- “Medical Error Reduction and Prevention,” by Thomas Rodziewicz, Benjamin Houseman, Sarosh Vaqar and John Hipskind, February 2024.
- “Medical Error — the Third Leading Cause of Death in the U.S.,” by Martin Makary and Michael Daniel, British Medical Journal 2016;353:12139.
- “The Safety of Inpatient Health Care,” by David Bates, Elizabeth Mort, et al, New England Journal of Medicine, January 11, 2023; 388:142-153.
- “Safety of Health Care in the Inpatient Setting,” by Matthew Scanlon and Kenneth Catchpole, New England Journal of Medicine, April 19, 2023; 388:1534-1536.
- “Your First Choice Is Your Most Important Choice,” by Allen Weiss, 4sightHealth, January 16, 2024.
- The Society of Thoracic Surgeons, STS Public Reporting, STS Public Reporting | STS.
- CDC Assisted Reproductive Technology (ART), December 10, 2024.
- Centers for Medicare and Medicaid Services, National Center for Reproductive Services, Data Collection, June 7, 2023.
- United Network for Organ Sharing (UNOS)
- “Transparency: Increase transparency in OPO, hospital and system performance by making more comparative data available publicly,” by United Network for Organ Sharing, 2023.
- Cancer Data and Statistics, December 3, 2024.
- NIH National Cancer Institute, Surveillance, Epidemiology and End Results Program, U.S. Department of Health and Human Services.
- NIH National Cancer Institute, Cancer Staging, U.S. Department of Health and Human Services.
- “Functional status, health problems, age and comorbidity in primary care patients,” by M. Wensing, E. Vingerhoets and R. Grol, Qual. Life Res. 2001; 10(2): 141-8.