October 24, 2018

No Time to Waste: Revolutionizing Healthcare Data Collection, Curation and Application
Healthcare data wants to be free, but it is oppressed. Entrenched oligarchs trap information within closed, centralized systems that prioritize revenue collection, misuse resources and tolerate medical error. Data gasps for breath as it fights to break into curated systems that produce insight.
Confronting intense technological impediments, frustrated clinicians struggle under to access information and apply it to patient care. Segmented data, poor communication and inefficient workflows diminish care effectiveness. At best, incremental improvements add clinical and operational functionality. They’re Band-Aids, not cures.
Rather than making care delivery better and easier, enterprise data systems overburden caregivers, exasperate everyone and harm patients. They serve themselves, not the people.
It doesn’t have to be this way.
Emerging cloud-based overlay technologies replicate real-time data onto HIPAA-protected, self-learning platforms. These platforms push data to where it delivers the most value. They enable designers to build apps that streamline operations, reduce waste and improve clinical outcomes. They make life easier for caregivers and consumers.
By 2020, healthcare knowledge will double (1) every 73 days. Even the most dedicated clinicians cannot keep up. Augmented Intelligence comes to the rescue. AI amplifies human capabilities by providing the right data at the right time to the right people. It generates insights. It nudges behaviors that support better clinical and operational outcomes.
 Open architecture, crowd-sourced solutions and engaged consumers will lead to better health and healthcare for all Americans. Data independence will help build a financially sustainable healthcare industry and a stronger economy.
Open architecture, crowd-sourced solutions and engaged consumers will lead to better health and healthcare for all Americans. Data independence will help build a financially sustainable healthcare industry and a stronger economy.
This is healthcare data’s future. There’s no time to waste embracing it.
It’s time to challenge the oligarchs repressing data flow. It’s time to support technologies that overwhelm closed data systems. Healthcare leaders must free data from its closed systems and the profit-first oligopolies (large EHR vendors) perpetuating the status quo.
Revolutions rise from hope and fury. Maintenance of the status quo is fear-based and unacceptable. Systems must evolve toward efficiency and create value. A new healthcare world, where data flows safely and freely, lies beyond the barricades. There’s no turning back.
Data Is as Data Does
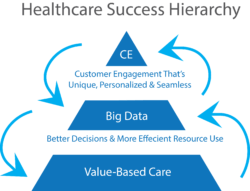 “Data” does not exist in isolation. It is the middle layer of a three-part success hierarchy. Healthcare data flows to and from this middle tier to inform value-based operations (the bottom tier) and fully-engaged customers (the top tier). The chart to the left captures these flows.
“Data” does not exist in isolation. It is the middle layer of a three-part success hierarchy. Healthcare data flows to and from this middle tier to inform value-based operations (the bottom tier) and fully-engaged customers (the top tier). The chart to the left captures these flows.
In the near future, post-reform, revolutionary healthcare organizations will use data to generate consistent high-quality outcomes, reduce performance variation and improve operational efficiency. Data inputs will flow to and from operations to improve care design and empower care delivery.
At the individual patient level, all relevant data from all sources will flow into algorithms that enable caregivers to optimize diagnosis and treatment. As data proliferates and analytics advance, individual genetic and environmental characteristics will lead to more personalized and less population-based therapies; more precision and less trial-and-error care.
At the individual disease level, all relevant information from all sources will flow into data systems advancing medical research and protocol development. Pricing and outcomes data will be transparent and available.
Unfortunately, getting the medical treatments “right” will not be sufficient to “win” in post-reform healthcare. Health organizations also must engage customers to gain their trust, confidence and loyalty.
Fully engaging customers requires a deep understanding of their needs. Revolutionary health organizations listen and respond to customer preferences. They deliver appropriate, user-friendly healthcare services with transparent prices that are unique, personalized and seamless. They create value, not friction. It’s happening now, at health systems with visionary leaders.
None of this should surprise. Consumer purchases drive 70 percent of the U.S. economy. Companies succeed and fail based on their ability to read and respond to consumers’ sentiments. Consumer-oriented companies spend billions of dollars on polling, focus groups and test marketing to enhance their product offerings.
Companies can’t tell consumers “what to do,” companies must “persuade.” Leading through persuasion is antithetical to most health company cultures where physicians dominate medical decision making. “Dr. Knows Best” doesn’t work for market-savvy baby boomers.
Big data analytics are essential for understanding consumer preferences. Collecting, measuring and evaluating consumer data drive strategic growth and customer acquisition. Companies use big data to design appealing products and services.
Healthcare has to overcome the control legacy systems maintain on data to unlock data’s transformative power. This will require displacement of healthcare’s data oligarchs that impede progress by clinging to suboptimal enterprise systems to maintain market control and sustain profitability.
Breaking the Technology Shackles
 Contrary to other industries, integrating new technologies has made healthcare more expensive. According to The Hastings Center, new medical technology and intensified use of existing technology are responsible for 40-50% of the annual increase in care costs. (10) Rather than streamlining and improving information access, Electronic Health Record (EHRs) often dissatisfy patients and providers, even after full implementation.
Contrary to other industries, integrating new technologies has made healthcare more expensive. According to The Hastings Center, new medical technology and intensified use of existing technology are responsible for 40-50% of the annual increase in care costs. (10) Rather than streamlining and improving information access, Electronic Health Record (EHRs) often dissatisfy patients and providers, even after full implementation.
The first rule of performance improvement is to fix systems before automating them. Healthcare organizations ignore this wisdom. Instead the industry has spent tens of billions of dollars automating a broken, fragmented system. EHR companies have profited enormously but failed to transform healthcare delivery.
As a result, healthcare data became siloed, stifled, retrospective and confined to checkboxes and drop-downs. These limitations contribute to suboptimal care, physician/caregiver burnout, burdensome workarounds, enormous financial waste and quasi-monopolistic behaviors by data oligarchs.
Patients suffer. A John Hopkins study in 2016 (2) calculated that more than 250,000-400,000 deaths annually result from medical error. Data systems play a role in many of those deaths. Patient Adverse Events (PAEs) result from errors in communications and diagnosis (3) orchestrated within EHRs.
Medication errors are commonplace, caused by computerized physician orders (CPOE) mistakes and flawed EHR documentation. Almost 70% of those mistakes influence patient care. (4)
Clinicians suffer. On average, physicians spend half of their workday entering data into EHRs and conducting clerical work and spend just 27% of their workday with patients. (5) Closed data systems have hijacked clinician workflow, pulling caregivers away from bedsides and higher-value work, turning them into data entry clerks and driving massive frustration and burnout.
Fifty-one percent of physicians report experiencing frequent or constant feelings of burnout in 2017, up from 40% in 2013. (6) Fifty-six percent of physicians blame documentation for that burnout, and 24% blame it on increased computerization working with EHRs. (7)
Frontline caregivers operate in a fog of data. There’s too much data but it’s not curated, accessible or prescriptive. Caregivers suffer from alert fatigue, both because of the cognitive overload associated with the amount and complexity of their work, and from the effort needed to differentiate informative from uninformative alerts. 
To overcome this fog and care for patients, clinician’s default to time-consuming workarounds that are inefficient, haphazard and fraught with peril. Medical errors are the third leading cause of death in the U.S. (8) A 2013 study estimated that 210,000 deaths per year relate to preventable harm in U.S. hospitals, up from a 1984 estimate of 98,000 annually. (9)
With limited options, health systems contract with a tiny number of powerful EHR providers at enormous cost with mediocre, often counter-productive, results. Both sides, however, benefit from reduced interoperability. Controlling patient data creates market power. A 2014 RAND study on EHRs highlights this market reality:
“The shift [to inter-operability] will be less welcome to large legacy vendors because it will blur the competitive edge they currently enjoy. Health care systems may be less-than-enthusiastic adopters because functional health information exchanges will make it easier for patients to see nonaffiliated healthcare providers or switch to a competing health care system.”
Data oligarchs not only restrict data flow, they use their power to block innovative companies from applying breakthrough IT capabilities and gaining market traction. They make incremental improvements on archaic, inefficient platforms. This gives the appearance of progress but thwarts transformation. Interoperability is for smaller, less important companies.
This is the monopolists’ prerogative. They aggregate wealth for themselves at society’s expense. They will continue until forced to stop.
The Manifesto for Data’s Future
Healthcare should serve patients and clinicians by liberating data flow, supporting innovation and pursuing better outcomes at lower costs. Specifically, health companies must embrace these principles to advance care delivery:
Provide Access: Support providers who keep patients first by making data accessible in real time, within the clinician’s workflow, to enable delivery of the right care at the right place at the right time.
Foster Insights: Place knowledge at the fingertips of frontline providers by incorporating the best retrospective and prospective clinical evidence and procedures.
Guarantee Data Rights: Award consumers individual rights over their own data by making it accessible as needed wherever they go, with appropriate privacy and security measures.
Pursue Open Data Flow: Allow data to flow securely between systems, so smart companies can find solutions for better clinical and operational performance through artificial intelligence and machine-based learning.
 In this new healthcare world, freed and curated data will solve complex problems. It will connect to cloud-based EHRs in real time to facilitate access, analysis and action. Moreover, combining data, infrastructure, people and communications creates a “hivemind,” where aligned groups of people collaborate to generate superior results efficiently. Effective and informed teams are always the best and most efficient problem-solvers.
In this new healthcare world, freed and curated data will solve complex problems. It will connect to cloud-based EHRs in real time to facilitate access, analysis and action. Moreover, combining data, infrastructure, people and communications creates a “hivemind,” where aligned groups of people collaborate to generate superior results efficiently. Effective and informed teams are always the best and most efficient problem-solvers.
Incremental, EHR-driven solutions have not and will not solve healthcare’s data challenges. Only radical improvement of data collection, curation and application can create the technology infrastructure necessary to power transformative improvements in care delivery, efficiency and customer engagement. Fortunately, other industries have already made this transformative leap.
(Read a quick description of the benefits for health systems that implement cloud-based data systems here.)
A Data Liberation Framework
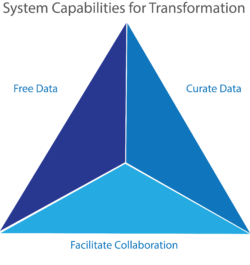
Like transportation, hospitality, retail and publishing, healthcare data must escape confining enterprise systems by accessing the cloud’s unparalleled security, interoperability, speed, access and analytic prowess. Data liberation through the cloud unlocks value for customers.
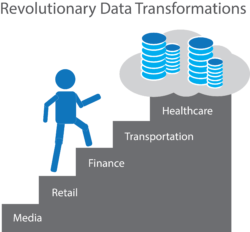 As industries mature, they decentralize to get closer to customers. Innovative practices become more democratic and proliferate at low costs. Workflows streamline and engage customers within aligned production and distribution platforms that tailor services to individual needs/preferences.
As industries mature, they decentralize to get closer to customers. Innovative practices become more democratic and proliferate at low costs. Workflows streamline and engage customers within aligned production and distribution platforms that tailor services to individual needs/preferences.
Consider Amazon’s contribution to retailing. Amazon collects, analyzes and acts on voluminous amounts of real-time customer data to tailor service offerings and create value for consumers. Amazon has created service platforms to delight customers, and the retail industry is radically different as a result.
New data platform companies are bringing these forward-thinking capabilities to healthcare. One example is MultiScale Health Systems, a company that has engineered a convenient, cloud-based solution that includes a real-time architecture, integrated clinical communication and collaboration framework, and problem-solving app development capabilities.
According to MultiScale’s CEO, Jim Harding, their “Hive” offering unleashes health data access and collaboration. Harding continues,
“Hive simplifies the way clinicians solve the problems that impact care quality, efficiency and costs. It reimagines clinical communication and collaboration with convenience and ease.”
Harding explains that “Problem-solving apps streamline the patient, operational, retrospective and predictive intelligence needed to solve potential problems before they happen. The Hive creates true data access by moving health data to a safe, secure cloud to enable real-time, curated data streaming.”
In hive architecture, securely-captured real-time EHR data integrates with real-time operational data to source problem-solving applications. These apps feed critical data and directions to frontline caregivers at the point of care. Radical re-engineering of healthcare data transforms healthcare delivery. Outcomes improve. Costs drop. Patients and clinicians engage.
Leading the Charge
 When data flows freely, care coordination improves dramatically – for health systems, caregivers and patients.
When data flows freely, care coordination improves dramatically – for health systems, caregivers and patients.
Providence St. Joseph Health (PSJH) aspires to become a value-based, consumer-centric healthcare organization. Learning from other organizations is a key part of the strategy. Their leadership team includes senior leaders from Microsoft, Amazon, Kaiser, United Healthcare, and T-Mobile. And their Chief Clinical Officer know how the problems they want to solve.
Dr. Amy Compton-Phillips, PSJH’s EVP & Chief Clinical Officer, tells potential partners and industry audiences that:
“I’m not even going to consider technology that makes my staff step out of their care workflow. That’s already too big of a problem. I’m looking for solutions that bring the data they need into that workflow.”
PSJH’s goal isn’t to replace workflows, it’s to make them better. Healthcare’s data revolution is happening now because computing power, digitized data, the cloud, AI and machine learning are propelling transformation of health system workflows.
Humans and machines make better decisions together. AI can improve outcomes 30-40% and reduce costs by up to 50%. (11) A September 2018 study, for example, found that a small group of AI-guided doctors made more accurate pneumonia diagnoses than both physicians without AI and AI alone. (12)
New companies and innovators have built convenient, consumer-grade apps to solve high-impact problems. These tools pull EHR data and clinical protocols together for step-by-step diagnosis and actions in time-sensitive health crises.
For the sake of their health organizations, leaders must acknowledge that the data status quo isn’t working and embrace today’s technologies that successfully transformed other industries. They must learn from peers who are trying new approaches and support those initiatives. By seeking out innovators who can bring these advances to healthcare, they can implement new approaches in their organization. Organizations will thrive when their leaders lean into the future today by setting health data free.
The infrastructure and systems exist to build a new world of healthcare data systems. As the healthcare industry rises up together to free and apply its data, the “Data Liberation” revolution will achieve higher quality, less cost, and improved outcomes.
Sources
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3116346/
- https://www.thehastingscenter.org/briefingbook/health-care-costs-and-medical-technology/
- https://www.hopkinsmedicine.org/news/media/releases/study_suggests_medical_errors_now_third_leading_cause_of_death_in_the_us
- https://journals.lww.com/journalpatientsafety/Fulltext/2013/09000/A_New,_Evidence_based_Estimate_of_Patient_Harms.2.aspx
- https://healthitanalytics.com/news/patient-safety-errors-are-common-with-electronic-health-record-use
- Annals of Internal Medicine, “Tethered to the EHR: Primary Care Physician Workload Assessment Using EHR Event Log Data and Time-Motion Observations,” September/October 2017
- Medscape Annual Survey 2017
- Medscape National Physician Burnout & Depression Report 2018
- https://www.cnbc.com/2018/02/22/medical-errors-third-leading-cause-of-death-in-america.html
- https://journals.lww.com/journalpatientsafety/Fulltext/2013/09000/A_New,_Evidence_based_Estimate_of_Patient_Harms.2.aspx
- https://www.eurekalert.org/pub_releases/2018-08/lu-pdd081518.php
- Frost & Sullivan, December 2015