June 10, 2020

Public Health and Healthcare in Post-COVID America: Innovative Solutions for a Healthier, More Prosperous Society
In the early 1900s, health epidemics ranging from cholera to typhoid plagued America’s increasingly crowded and polluted cities. Public health services emerged during this time to manage the onslaught of these virulent infections.
Early countermeasures focused on “outside sources” of disease, including quarantining afflicted (usually immigrant) communities and rejecting diseased newcomers at Ellis Island. Ultimately, however, more effective interventions addressed root causes in public health.
In a wave of modernization, governments funded public infrastructure projects for clean drinking water and better sewer systems. Cities began regular garbage removal and insect spraying. Health inspectors ensured hygiene standards at workplaces and crowded apartment buildings. The FDA, founded in 1906, reinforced the importance of child nutrition and nurturing through public education campaigns.
These progressive measures focused on important living and environmental conditions – now called social determinants of health (SDoH). They helped reduce the virulence of disease while also improving life quality, expanding education, lowering infant mortality and raising life expectancy.
In this century, America once again finds itself confronting a dire need for better public health services. Total health spending represents over 18% of GDP even as chronic disease rates increase and health status metrics lag those of other advanced economies. Relative to its peers, the U.S. spends less on social care. Social barriers to health among disadvantaged populations and communities underlie America’s dismal health statistics.
COVID-19’s disproportionate impact on vulnerable populations has made the nation’s social disparities even more apparent. Social determinants such as economic status, access to transportation and basic care services, housing and food security, health literacy and age, race and chronic illness have accelerated COVID-19’s spread and lethality.
A potential positive outcome from this crisis is the opportunity to systematically address SDoH at national scale. Numerous organizations are already applying innovative and cost-effective SDoH solutions. The challenge is to coordinate and scale their efforts and maximize their impact. This will require the removal of major barriers to better healthcare services, including changing the way we value and pay for care.
The Outsized Impact of Social Determinants of Health
Research indicates that social factors and lifestyle behaviors determine approximately 60% of an individual’s health status. Clinical care accounts for only 10-15% of health status.
Clinical care services, particularly acute treatments, account for the vast majority of America’s healthcare expenditures. The inverted relationship between health spending and sources of health status explains why America’s expansive healthcare spending yields suboptimal health outcomes. Other advanced economies have more balanced spending between healthcare and social care. As a consequence, their health status indicators surpass those of the United States.
Many Medicare and Medicaid beneficiaries, in particular, confront major social barriers to managing their health. The following charts illustrate how SDoH afflict these populations.
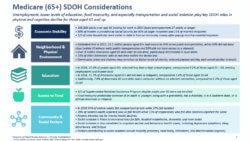
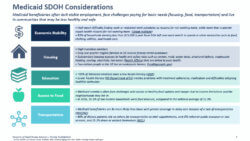
Vulnerable population are typically older, sicker, poorer and have fewer resources. Many lack adequate housing and food, find transportation difficult and suffer from mental health conditions or social isolation. The chronically ill, the elderly, and smokers, in particular, are at higher risk of premature death.
Not surprisingly, COVID-19 has preyed on these groups. Overall, the U.S. has 5% of the world’s population but has absorbed 30% of COVID-19 deaths. The elderly, dispossessed and/or those with chronic disease constitute the majority of COVID-19’s victims.
Barriers That Impede or Limit SDoH Interventions
CMS and state health agencies have taken a lead in addressing SDoH more comprehensively. Medicare Advantage and managed Medicaid programs create financial incentives for plan sponsors to address members’ health and wellness needs. While these initiatives are promising, the following characteristics of U.S. healthcare limit implementation of well-established practices for managing the health of large populations.
MISALIGNED INCENTIVES Fee-for-Service (FFS) payment models encourage the delivery of fragmented and transactional healthcare services, often in centralized, high-cost facilities. Healthcare services reactively treat illness, disease and injury. There is minimal payment for proactive services that prevent disease, manage chronic illness or address emerging mental illness.
LACK OF ACCESS TO PRIMARY, PREVENTIVE AND BEHAVIORAL CARE Populations with high social barriers to health often lack access to primary, preventive and behavioral care services. Consequently, many vulnerable populations fail to address health issues before they become more problematic. Effective primary care enhances wellness and reduces the need for costlier interventions.
LACK OF HOLISTIC / COMMUNITY-BASED APPROACH Complex health problems require coordinated, holistic care delivery. This rarely occurs. Providers best address SDoH challenges by engaging patients and addressing their health and social care needs within a trusting provider-patient relationship.
A NEED FOR ROBUST TECHNOLOGY, DATA SHARING AND ANALYTICS Most EHR systems and tools impede data sharing and patient engagement. They focus instead on controlling patient data and optimizing revenue collection. Robust data and analytics can help identify and engage vulnerable individuals.
AVAILABILITY OF RESOURCES Low-income communities often lack the resources, services and infrastructure to address SDoH effectively. Solutions can be difficult to scale and/or coordinate without adequate funding, technology and operational expertise.
Investments and Innovations
As payment models incentivize care management, investment and experimentation in SDoH initiatives is growing. Private organizations are taking multiple approaches in developing SDoH solutions.
The following chart illustrates the sizable number of early-stage and established organizations addressing the specific categories of social care.

Implications for Payers and Providers Investing in SDoH Programs
Although numerous innovative organizations are addressing SDoH, they typically offer point solutions for specific social barriers. Real progress in addressing social care needs requires coordinating these types of point solutions. Large providers and payers are well-positioned to assemble and operate these services within cohesive care delivery platforms that exhibit the following features:
- Better data collection and analytics to understand member populations and target communities and individuals, improve patient identification and tracking.
- Adoption of predictive models that address care needs and gaps.
- Deeper engagement with members / patients to understand and address holistic needs, improve adherence, and drive healthy behaviors and lifestyles.
- Broader integration in the larger social support infrastructure while filling gaps where necessary.
- Investment in business capabilities and processes that enhance information sharing, improve workflow, reduce administrative burden and facilitate collaboration between partners in shared-risk arrangements.
To demonstrate their value, SDoH solutions will need to deliver positive investment returns over time. Cost savings and improved health outcomes will help gain executive and policymaker buy-in to devote more resources and utilize SDoH solutions more broadly.
Targeted investments in care management models generate savings over 3-5-year horizons. Payment models must accommodate these longer return horizons for care management programs to succeed. Again, large providers and payers are well-positioned to make coordinated SDoH investments and assess their success.
Developing effective ROI metrics is difficult but not impossible. For example, IU Health has developed the Healthcare Economic Efficiency Ratio (HEERO), which gauges actual spending on patient care against expected spending on patient care based on claims data for patients attributed to Medicare Advantage health plans or a Medicare accountable care organization.[1]
A Holistic, Scalable Approach: Oak Street Health
Oak Street Health, a care provider for Medicare and Medicaid beneficiaries, opened its first care center in Chicago’s Edgewater neighborhood in 2013 and has since expanded to 55 centers in 8 states. The founding team established Oak Street to address disparities in quality of care and access to care in under-served neighborhoods, and to “rebuild healthcare as it should be.”

Oak Street’s model is consistent from center to center. As CEO-founder Mike Pykosz notes, “Healthcare infrastructure might be local, but the clinical needs of a diabetic are the same everywhere. We pick neighborhoods that are underserved and build our centers from scratch with one clinical model for how we treat patients and a common digital IT platform.”
Oak Street patients struggle with a litany of social barriers to health, ranging from chronic conditions and low economic status to housing and food insecurity. The population is unaccustomed to accessing preventive care and typically relies on costly ER visits. Pykosz says, “We put a lot of effort into community outreach and educating people on the importance of preventive care and regular primary care.”
Oak Street’s at-risk or capitated business model is predicated on taking the savings from reduced ER visits and hospitalizations and applying those resources to lower-cost care solutions that improve overall health status. This incentivizes Oak Street to treat patients holistically with frequent check-ups and interventions that address social barriers such as a lack of food, housing or transportation.
With the onset of COVID-19, Oak Street has transitioned almost all of its in-center care to virtual and tele-care visits. “We’re doing more provider visits a day than we did two months ago,” Pykosz says, “all virtual.”
Oak Street calls their patients multiple times a day, checking on their condition, directing them to seek in-person care or testing if necessary, and educating them on the latest COVID guidelines. Oak Street also delivers meals so that patients stay fed and safe in their homes.
Pykosz credits their capitated payment model for Oak Street’s operating flexibility and capacity to focus exclusively on members’ health and social care needs.
“We’re not worried about what’s reimbursable and whether there’s a code to do something. It’s harder for fee-for-service groups to invest in what patients actually need.”
Conclusion: Meeting the Surging Need for Quality Care
COVID-19 has accelerated the need for effective SDoH solutions.
Medicaid programs are already stretched thin, but their enrollment will grow with the prolonged economic downturn. At the same time, the number of uninsured requiring uncompensated care also will increase.
As the COVID-19 storm intensifies, SDoH solutions that decrease overall care costs and improve health outcomes are imperative. A keen understanding of local markets is critical in selecting the right solutions. Yet, the best solutions will also be scalable across many communities and populations.
As Oak Street Health demonstrates, innovative and effective solutions for managing the care of populations emerge when payment models incorporate prepayment and financial risk. This alignment between payment and outcomes enhances innovation, flexibility and coordination in meeting the diverse needs of vulnerable populations.
America won’t change the way it delivers care until it changes the way it pays for care. When payment and desired outcomes align, the potential for cost savings and improvement in health metrics drive investment in innovation and holistic services across the industry.
Sources:
Co-authors:
 Court Houseworth co-leads Cain Brothers Managed Care advisory practice. Mr. Houseworth joined Cain Brothers in 2004 and has over 30 years’ experience advising both public and private companies in a variety of merger and acquisition, capital raising, and strategic advisory transactions, as well as valuations and nonprofit conversions. Mr. Houseworth’s notable transactions include the sale of Kids Care Dental & Orthodontics to RiverGlade Capital, the sale of Pathways to Atar Capital, the acquisition by Blue Shield of California of Care1st Health Plans, Blue Cross of Northeastern Pennsylvania’s merger with Highmark, the sale of Avesis, Inc. and the sale of Premier Access Insurance Company to The Guardian Life Insurance Company of America, the sale of Foundations Recovery Network to N Pritzker Capital Management, and the sale of Centerre Healthcare to Kindred Healthcare.
Court Houseworth co-leads Cain Brothers Managed Care advisory practice. Mr. Houseworth joined Cain Brothers in 2004 and has over 30 years’ experience advising both public and private companies in a variety of merger and acquisition, capital raising, and strategic advisory transactions, as well as valuations and nonprofit conversions. Mr. Houseworth’s notable transactions include the sale of Kids Care Dental & Orthodontics to RiverGlade Capital, the sale of Pathways to Atar Capital, the acquisition by Blue Shield of California of Care1st Health Plans, Blue Cross of Northeastern Pennsylvania’s merger with Highmark, the sale of Avesis, Inc. and the sale of Premier Access Insurance Company to The Guardian Life Insurance Company of America, the sale of Foundations Recovery Network to N Pritzker Capital Management, and the sale of Centerre Healthcare to Kindred Healthcare.
 Kyle Stern is a Managing Partner at HealthScape Advisors. He assists health plans, specialty care companies, and ancillary carriers in a variety of areas including new business and market development, cost reduction, business process improvement, and financial and data analytics. He also works closely with private equity firms in their pursuit and evaluation of investment opportunities in emerging growth markets.
Kyle Stern is a Managing Partner at HealthScape Advisors. He assists health plans, specialty care companies, and ancillary carriers in a variety of areas including new business and market development, cost reduction, business process improvement, and financial and data analytics. He also works closely with private equity firms in their pursuit and evaluation of investment opportunities in emerging growth markets.





