June 4, 2024

Site-Neutral Payment and the Battle for Healthcare’s Soul
In a remarkable and surprising show of bipartisanship, the U.S. House of Representatives passed the “Lower Costs, More Transparency Act” December 11, 2023, by an overwhelming 320-71 vote. Avoiding hyperbole, the Act lives up to its name. It seeks to equalize Medicare payment for the same drugs administered in the same way whether in hospitals or in doctors’ offices. Seems reasonable but the American Hospital Association (AHA) begs to differ.
Medicare pays two-to-three times more for administering the same drugs in hospital-owned facilities (including doctors’ offices) than in independent doctors’ offices. This practice creates financial incentives for hospitals to acquire physician practices, and so they have. The Medicare Payment Advisory Commission (MedPAC) reports that Medicare paid hospital-based prices for over half of all chemotherapy drugs administered in 2021, up from a third in 2012.
The Congressional Budget Office estimates that site-neutral payment for administering drugs will save Medicare more than $3.7 billion over 10 years. It also would generate significant savings for private health insurers. According to Kaiser Family Foundation research, private insurers pay hospitals twice as much as Medicare does for the same services. Let’s not forget consumers. The Act reduces copays for Medicare beneficiaries by $40.
Saving money by eliminating irrational pricing variation is elemental to good policy creation. That’s why the Lower Costs, More Transparency Act is receiving such widespread support. Of course, creating savings in one pocket creates a hole in another. Aggrieved hospitals depend upon irrational payment policies to sustain their stagnant business practices. They’re howling at Congress to protect the status quo.
Healthcare’s Anti-Innovation Mindset
In a blistering letter to Congressional leaders, the AHA blasted site-neutral payments for administering drugs. They insist that the House bill ignores core operating realities and will inflict grave harm on hospitals. Their sky-is-falling analysis basically accuses Congress of putting American consumers in danger.
Congressional action on this issue, along with the continued government underfunding of hospital and health systems, puts patient care at risk, particularly in rural and undeserved areas.
The AHA’s rhetoric got even hotter after a March 14, 2024, editorial in the Washington Post endorsed the Act. In a blog post to “set the record straight,” the AHA president and CEO described the Post’s editorial as “deeply flawed and poorly timed.” Rick Pollock ended his blog by lecturing Congress to stop putting “patient access to care in jeopardy.”
What truly worries the AHA, however, is that Congress will broadly apply site-neutral payment to treatment activities beyond drug administration. MedPAC has identified 57 potential applications for site-neutral payment that would save Medicare $150 billion over 10 years.
Here’s the problem with the AHA’s logic. Paying more for identical service provision is the antithesis of innovation and value creation. Gaming payment formularies is a value-depleting activity. Hospitals and health systems aren’t innovating on service delivery because we’re paying them not to innovate.
Disruption 101
Harvard Business School professor Clay Christensen is the undisputed guru of disruptive innovation. Christensen’s pathbreaking work explains how disruptive innovations create value by finding new and better ways to solve customers’ “jobs to be done.” As the AHA is discovering, resisting innovation is like resisting gravity. It takes enormous effort and ultimately comes crashing down to earth. No one innovates by charging more for existing services.
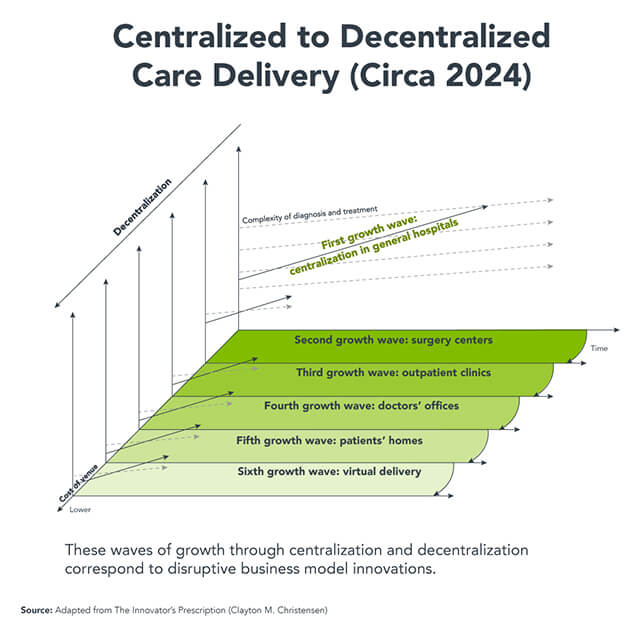
In 2009, Christensen published “The Innovator’s Prescription,” which applies his theories on disruptive innovation to the healthcare industry. Christensen’s analytic brilliance lies in his ability to see patterns within chaotic and tumultuous markets, distill their implications and apply them proactively. A consistent theme in Christensen’s work is the interplay between centralization and decentralization as industries grow and mature:
…in the beginning stages of nearly every advanced industry, the initial products and services are complicated and expensive. Disruption then “democratizes” these, by making products and services that are simpler and more affordable.
Staging is an essential component of Christensen’s centralization-decentralization framing. “Modern” technologies bring quantum improvements in the quality, cost and speed of production. This is when industries move from “Stage Zero” to “Growth Wave One.” The investments in technology and expertise to achieve these quantum-level improvements are expensive. Consequently, it is more efficient and cost-effective to centralize production.
 Over time, industry products and services standardize, even commoditize. Disruptive innovators attack the high costs and inconvenience of centralized operations. In Growth Waves Two, Three and beyond, industries begin to decentralize in order to lower costs, increase efficiency and improve customer experience. In applying these growth waves to medical care, Christensen illustrates how disruptive innovations are fueling decentralized delivery of healthcare delivery:
Over time, industry products and services standardize, even commoditize. Disruptive innovators attack the high costs and inconvenience of centralized operations. In Growth Waves Two, Three and beyond, industries begin to decentralize in order to lower costs, increase efficiency and improve customer experience. In applying these growth waves to medical care, Christensen illustrates how disruptive innovations are fueling decentralized delivery of healthcare delivery:
- Stage Zero: Doctors, nurses and family took care of the sick in homes.
- Growth Wave One: Patients go to general hospitals where doctors and nurses provide care.
- Growth Wave Two: Procedures that once required hospitalization can be performed in ambulatory clinics and surgery centers.
- Growth Wave Three and Beyond: Procedures that once required going to an ambulatory clinic or surgery center can be done in doctors’ offices.
What’s unusual about healthcare is the extent to which the industry’s business strategies have stalled in Growth Wave One, which emphasizes centralized service delivery. In healthcare, disruptive innovations haven’t led to lower prices like they have in other industries (e.g., retail shopping, hospitality, banking, transportation). Healthcare’s strategic stagnation occurs because health systems insist on receiving higher hospital-based payments for procedures delivered in lower-cost settings, including ASCs and physicians’ offices.
Fighting against innovation, value creation and transparency is a soul-destroying endeavor. The industry’s increasingly shrill warnings are falling on deaf ears. The world, as illustrated by House passage of the Lower Costs, More Transparency Act, is moving forward despite industry protests.
Although it’s daunting to contemplate, the right response for providers is to embrace site-neutral payment and use innovation to spur waves of Growth Waves that deliver better outcomes at lower costs with great customer service. Ride the wave to achieve better outcomes and happier customers. This is a soul-enriching endeavor.
Do health systems really have another choice?





