May 13, 2021
Stigma vs. Science: Overcoming Opioid Addiction with Evidence-Based Treatments and Services
Before COVID, the opioid crisis was America’s most dire public health challenge. Though it has receded from the headlines, that crisis has not gone away. In 2020, the opioid-related death rate spiked dramatically.
Listen to the authors discuss this article on the Cain Brothers Podcast, House Calls, available on iTunes, Spotify, and Google Podcasts.
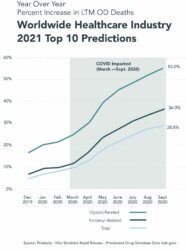
Between September 2019 and September 2020, 90,000 Americans died from drug overdoses. More than 70% of these overdose deaths were opioid-related. This represents a 28.8% increase over the previous year, the worst on record. [1]
Since 1999, the opioid epidemic has killed almost 500,000 Americans. The death rate is accelerating. More than half of opioid overdose deaths have happened in the past five years. [2]
Historical approaches to addiction treatment have proven insufficient. Despite rising appreciation for the clinical, societal and emotional challenges that shape opioid addiction, stigma remains a barrier to treatment.
Promising research suggests a holistic blend of evidence-based approaches can slow the death rate and enable more of the afflicted to lead healthier, more productive lives. Unfortunately, the current need for holistic services far outpaces supply.
There is hope. Medication-assisted treatment programs are expanding; new care delivery modes are emerging; access is improving; and the highly fragmented addiction treatment sector is beginning to consolidate.
Sobriety, Stigma and Addiction Treatment Failure
Forty years ago, Nancy Reagan used her position as First Lady to launch the “Just Say No” campaign as part of the larger War on Drugs. In the late 1980s, Partners for a Drug Free America began its long-running “This is Your Brain on Drugs” campaign.
Abstinence campaigns and sobriety-focused programs have proven no match for the powerful addiction of opioids. Drug overdoses are now the leading cause of accidental death in the U.S. Opioids, including prescribed or illicitly obtained drugs like Oxycontin and illegal narcotics like heroin and fentanyl, are largely to blame.
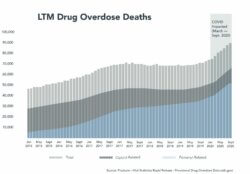
*Fentanyl-related represents synthetic opioids excluding Methadone.
Opioids are more dangerous and addictive than alcohol or cannabis. Fentanyl, a synthetic opioid, is considered 50-to-100 times more addictive than heroin. While overdose deaths due to prescribed opioids and heroin are slowing, fentanyl-related deaths rose more than 55% in the twelve-month period ending in September 2020.
Left untreated, addiction is devastating for addicts and families. Beyond the suffering and death, substance use disorder (SUD) costs America $600 billion [3] annually. This includes lost work days, incarceration and treatment for overdose victims in emergency rooms and hospitals.
Social stigma is a barrier to better care. While the American Medical Association classified addiction as a disease in 1987, too many people still see drug addiction as a moral failing and something to hide in the shadows. Addicts and families may lack the information, resources and support they need to seek help.
Such stigma also inhibits treatment. Clinical evidence shows that programs combining a holistic and integrated mix of psycho-social support, clinical therapy and medication-assisted treatment (MAT) are more effective for many addicts. MAT incorporates medications such as methadone, buprenorphine, or naltrexone to reduce withdrawal symptoms and cravings. Despite these benefits, sobriety-focused programs often forgo that form of treatment because it substitutes one drug for another. Only 10-20% of people with opioid addictions receive MAT. [4]
In contrast, consider the acceptance and effectiveness of nicotine patches. Smokers may remain addicted to nicotine, but the patch reduces the harmful effects caused by tobacco inhalation.
Mental illness is another contributing factor in addiction. Nearly half of the 20 million people diagnosed with SUD suffer from mental illness. Many likely turn to opioids to self-medicate. While fewer than 15% of SUD sufferers receive treatment, that number drops to 8% for those with co-occurring mental health challenges. [5]
COVID has compounded these difficulties. During the pandemic, isolation intensified loneliness and left many people without social support or ready access to treatment. Alcohol and drug use skyrocketed as a result, leading to more opioid- and alcohol-related deaths. [6]
The pandemic also disrupted the supply of treatment medications. The temporary shutdown of harm reduction programs, like needle exchanges and safe injection sites, increased health risks.
Payers and stakeholders should promote any program or modality that assists addicts in returning to their daily lives. Instead of putting up barriers to treatment, they should eliminate hurdles and assist users seeking treatment by steering them to programs most appropriate to their specific needs.
Coverage and treatment must also take into account the difficulty of recovery. The relapse rate for substance abuse disorders is typically 40-60%. For heroin users, it’s as high as 90%. [7] Instead of viewing relapse as a failure, effective programs recognize it is as part of the treatment journey.
Treatment Evolution and Innovation

Addiction treatment programs are not new. In the U.S., they date back to the 1700s with the advent of sobriety circles and sober houses. Despite best intentions, the history of addiction treatment is marked by missteps and misunderstanding. Today, there is more reason for hope.
The passage of the Mental Health Parity and Addiction Equity Act of 2008 (MHPAEA) was a milestone achievement. This legislation requires group health insurers and group health plans to provide the same level of care for SUD and mental health patients as they do for patients requiring medical and/or surgical care. Additionally, new programs and waivers have increased treatment options for individuals covered by Medicaid.
As coverage for SUD has improved, clinical treatment programs have advanced. They can be categorized into three groups.
Sobriety-Based Programs
Sobriety-based programs have a long history in treating addiction. Founded in 1935, Alcoholics Anonymous (AA), the original 12-Step program, addresses alcohol addiction through fellowship and spiritual support. Today, AA has over 2 million members within 118,000 groups worldwide. [8]
Established in 1953, Narcotics Anonymous (NA) applies AA programming to help people with substance use disorders. It hosts over 70,000 weekly meetings worldwide. [9]
Today, most addiction treatment programs are not limited to traditional sobriety counseling alone. Many have adopted medication treatment to support early detoxification and also incorporate cognitive behavioral therapy (CBT) and motivational enhancement therapy (MET). These programs often rely on community reinforcement to reduce social encouragement to abuse.
Medication-Assisted Treatment Programs (MAT)
MAT programs are increasingly prevalent for opioid addiction. They incorporate the use of medications such as buprenorphine, methadone and naltrexone. These drugs reduce cravings and restore the ability to function in daily work and life without producing a “high.”
Around 23% of publicly funded and more than 50% of private-sector treatment programs prescribe medication. [10]
Hybrid Programs
Today, innovative programs employ a holistic model that combines traditional sobriety, MAT, psycho-social therapy and recovery support. The Hazelden Betty Ford Foundation in Minnesota has been a leader in collecting, analyzing and sharing their research into these holistic treatment approaches. [11]
Early evidence indicates that combining medication with cognitive behavioral therapy (CBT), contingency management and supportive counseling helps people with opioid use disorders lower cravings, ease withdrawal, reduce relapses and extend recovery.
Results vary depending on the type of medication, the delivery process, setting, and the level of follow-up care. For patients with less severe addictions, MAT alone may be sufficient. For others, recovery is a long-term if not life-long process that may combine medication, counseling, 12-Step programs and care coordination.
COVID-Related Treatment Innovations
Many addiction treatment providers responded to the COVID shutdown by adopting a number of innovations. Some incorporated telehealth services and virtual platforms for individual and group therapy. [12] Many reduced barriers to MAT access by allowing take-home medications. In Colorado, mobile clinics already bring addiction treatment services to rural communities. Successful innovations may be adopted more broadly.
Combining virtual care services with traditional care delivery shows real promise in enhancing access and improving retention numbers, especially for patients at some distance from treatment centers. Progress is also being made expanding access through regulatory changes. 31 states have now applied for waivers to expand opioid addiction treatment services to Medicaid members. [13]
Treatment Alignment

With over 16,700 treatment clinics nationally, the substance-abuse treatment sector is highly fragmented and ripe for expansion, growth and consolidation. Consolidation of regional platforms and de novo growth could improve access and promote care standardization at scale.
Optimal platforms could offer a clinically-driven, holistic approach to addiction and mental health treatment, tailored to individual needs, with robust coordination across referral networks, social support organizations and acute, long-term care providers. Services might include the following:
- Inpatient detoxification and rehabilitation
- Residential treatment programs
- Partial hospitalization and intensive outpatient programs
- Dual diagnosis and mental health treatment (inpatient and/or outpatient)
- Outpatient behavioral treatment (CBT, family therapy, motivational interviewing, etc.)
- Medication-assisted treatment
- Medication management
- Outpatient detoxification
- Specialty treatment programs
- Health and wellness programs
- Broad affiliation / coordination with health systems and treatment partners
- 12-Step / group-therapy programs
- Sustained recovery programs
- Teletherapy services
- Peer counseling / long-term engagement
As research and evidence accumulates, public and private insurers will increasingly steer beneficiaries to service providers with scale, efficiency and best-practice treatment programs.
Addiction is a complicated disease, and a one-size fits all approach isn’t the solution. Networks of scaled, sophisticated providers could meet the nation’s urgent need for evidence-based treatment. By eliminating barriers, improving access, optimizing processes, accelerating intake and tailoring programs to individual needs, leading providers enable more individuals to receive high-quality care, achieve positive outcomes and return to their daily lives.
The following companies exemplify that approach.
Pyramid Healthcare, founded in 1999, combines behavioral health and medication and treatment services for people with co-
occurring mental health disorders. Pyramids’ services encompass adults and teens in all stages of addiction. They include outpatient treatment, inpatient rehab, drug and alcohol detox programs, medication management, dual diagnosis treatment programs, specialty treatment programs, outpatient mental health treatment and teletherapy services.
BayMark Health Services, based in Lewisville, TX, is a leading provider of MAT for opioid addiction across the U.S. and Canada. Its evidence-based programs rely on medication and counseling to reduce cravings, withdrawal symptoms and obsessive thoughts associated with opioid addiction. Additional services provide support and structure to avoid relapse and improve health.
Summit BHC, founded in 2013, operates a network of behavioral health centers throughout the U.S. Programs are largely sobriety focused and include inpatient acute psychiatric services. Summit also offers patient hospitalization, detoxification, health and wellness, residential chemical dependency and intensive outpatient services, as well as dual diagnosis treatment.
Conclusion: Addressing and Overcoming a Public Health Catastrophe
Despite incalculable suffering, the opioid crisis shows no signs of abating. “Just Say No” moralism, persistent stigma toward the afflicted, increasingly addicting variants, a dearth of comprehensive research, and lack of scale for evidence-based approaches have impeded treatment and recovery for millions of Americans.
It is time to battle opioid addiction by leveraging evidenced-based research and deploying effective clinical, therapeutic, care delivery, and social support tools, systematically.
As a chronic and too-often fatal disease accompanied by complicated societal and behavioral health challenges, opioid addiction will be a long-term or even life-long health condition for many. Promising new treatment approaches offer real hope for restoring lives and health.
Addiction services represents a large addressable market. Innovative providers have tremendous opportunity for growth while filling a deep societal need for lifesaving and life-changing care.
Sources
- https://www.cdc.gov/nchs/nvss/vsrr/drug-overdose-data.htm
- https://www.cdc.gov/drugoverdose/epidemic/index.html
- https://www.drugabuse.gov/publications/principles-drug-addiction-treatment-research-based-guide-third-edition/preface
- https://www.samhsa.gov/data/sites/default/files/reports/rpt29392/Assistant-Secretary-nsduh2019_presentation/Assistant-Secretary-nsduh2019_presentation.pdf
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4695242/
- https://www.cdc.gov/media/releases/2020/p1218-overdose-deaths-covid-19.html
- https://www.drugabuse.gov/publications/drugs-brains-behavior-science-addiction/treatment-recovery
- https://med.stanford.edu/news/all-news/2020/03/alcoholics-anonymous-most-effective-path-to-alcohol-abstinence.html
- https://www.tpoftampa.com/brief-history-of-narcotics-anonymous/
- https://www.healthaffairs.org/do/10.1377/hblog20180927.51221/full/
- https://www.hazeldenbettyford.org/education/bcr/addiction-research/medication-assisted-treatment-opioid-addiction-wp-1017
- https://www.hazeldenbettyford.org/education/bcr/addiction-research/telehealth-addiction-treatment
- https://store.samhsa.gov/sites/default/files/d7/priv/medicaidfinancingmatreport_0.pdf
Co-author
 Erika Haanpaa is a Director in the Firm’s Corporate M&A Advisory practice. Ms. Haanpaa joined Cain Brothers in 2018 and brings 10 years of investment banking and advisory experience, working with both private and public companies in a variety of merger and acquisition, capital raising, and capital markets transactions. Prior to joining Cain Brothers, Ms. Haanpaa was a Vice President in the Consumer and Retail Investment Banking Group at KeyBanc Capital Markets. Ms. Haanpaa’s prior experience also includes transaction advisory in KeyBanc Capital Markets’ Mergers and Acquisitions and Real Estate Investment Banking Groups. Ms. Haanpaa received her BS in Management from Purdue University and her MBA from the Kelley School of Business at Indiana University.
Erika Haanpaa is a Director in the Firm’s Corporate M&A Advisory practice. Ms. Haanpaa joined Cain Brothers in 2018 and brings 10 years of investment banking and advisory experience, working with both private and public companies in a variety of merger and acquisition, capital raising, and capital markets transactions. Prior to joining Cain Brothers, Ms. Haanpaa was a Vice President in the Consumer and Retail Investment Banking Group at KeyBanc Capital Markets. Ms. Haanpaa’s prior experience also includes transaction advisory in KeyBanc Capital Markets’ Mergers and Acquisitions and Real Estate Investment Banking Groups. Ms. Haanpaa received her BS in Management from Purdue University and her MBA from the Kelley School of Business at Indiana University.