April 11, 2023
Still Time For a Healthcare Industry Reinvention (Part 2)
Editor’s Note: This is Part 2 of a multi-part series on healthcare revolution. This article builds on Part 1, which you can read here.
Based on a 23-year career as a solo-practicing rheumatologist, internist and geriatrician, followed by 18 years as president and CEO of a 715-bed, two-hospital healthcare system, I recently shared thoughts about the current stressed healthcare system including profit margin squeeze, patient’s needs and suggested options of subdividing care into acute, urgent, and elective facilities. The bottom-line quote from the Mayo Brothers, “The Patient’s Needs Come First,” is my declaration to use prevention as the way to focus our attention to those we serve.
Recognizing and Addressing the Challenge
Patients’ healthy life expectancy should be the focus of the healthcare industry, communities, employers and governments. People live longer, happier and healthier lives when productivity improves and costs decrease.
The U.S. life expectancy at birth is at the lowest level since 1996. The 0.9-year drop in life expectancy in 2021 and the 1.8-year drop in 2020 were the biggest two-year declines in life expectancy since 1921-1923. The current decline — 77.0 to 76.1 years — demands a change, whether welcome or not. [1]
Our nation’s metrics are embarrassing compared to other countries. Consider just one. “Average life expectancy in Costa Rica has steadily increased from 55 years in 1950 to 81 years today — far outpacing the U.S. Even more notable: the country has achieved this success while spending far less than the U.S. as a share of income which is already lower than ours.” [2] This Central American country is about the size of West Virginia and has a vast and sparsely populated terrain in addition to a few cities. Older adults, even in rural areas in Costa Rica, do well compared to our nation. Opportunities abound to learn from others. [3]
Physicians, Non-Physician Caregivers and Community Responses
 Incumbents never welcome disruption. Currently, volume drives the U.S. health payment system. Profitability is proportional to the number of sick-care encounters. The more visits to a physician or hospital parallels greater demand for pharmaceuticals and devices/implants. Higher volume translates into increased insurance premiums the following year, of which the insurance company receives a percentage.
Incumbents never welcome disruption. Currently, volume drives the U.S. health payment system. Profitability is proportional to the number of sick-care encounters. The more visits to a physician or hospital parallels greater demand for pharmaceuticals and devices/implants. Higher volume translates into increased insurance premiums the following year, of which the insurance company receives a percentage.
Prevention is not top of mind and redirecting patients to focused factories would be anathema for local hospitals and physicians — both groups are volume dependent.
Offloading outpatient care to lower-cost caregivers — Walmart, CVS, Walgreens, and others — cuts into the work and profit of primary care physicians in independent and health-system-owned group practices. The same with telemedicine. Nurse practitioners and physician assistants, under the supervision of a physician, can bill Medicare at 85% of a physician’s fee with modest restrictions. This positions them to both help and compete with primary care physicians. [4] New entrants — companies and non-physician caregivers — will lower overall costs. That’s a good thing unless you are the traditional medical office or primary care physician being replaced.
Communities have pride in their local healthcare system, especially since it is typically the largest or second largest employer in town. Rethinking where to find urgent or elective care that would require some travel would be a complete mindset change, like the change in shopping after big box stores and online shopping matured. Some communities with abundant resources may support under-utilized healthcare (and retail) facilities but keeping afloat without adequate volume is challenging.
Conditions change and with the importance of health and well-being, patients’ mindsets can evolve to include some travel for urgent and elective care. For its 1.1 million employees, Walmart and other large national employers instituted a Centers of Excellence Program that directs patients with non-acute episodic needs to health institutions that treat them cost-effectively with positive outcomes.
Patients and a companion have 100% of the cost for surgery plus travel expenses for certain spine, cardiac, organ transplants, hip/knee replacements, weight loss surgery and fertility. Walmart also offers a record review for cancer care at a handful of selected healthcare systems across the nation. [5] Since cancer care requires both an accurate diagnosis and usually prolonged treatment, the selected health system develop protocols for a patient that are implemented conveniently for the sufferer.
Rural healthcare is already struggling financially and faces greater threat. Small rural hospitals are failing. Addressing the three levels of medical need with a centralized system might serve patients better than every community trying to be everything to everyone.
Cities with duplicative and redundant services could provide better centralized care more efficiently for a wider geographic area. Changing the “pride in ownership” will require more pain, namely financial pressure, but the reward for patients will be better objective outcomes. Coopetition will facilitate the transformation.
Something has got to give. With increased transparency, patients have never been better informed, and they are already seeking specialized care with better outcomes. Transportation and virtual audio/visual communication is easier than ever before, accelerating change for complex patients.
Healthcare System Evolution
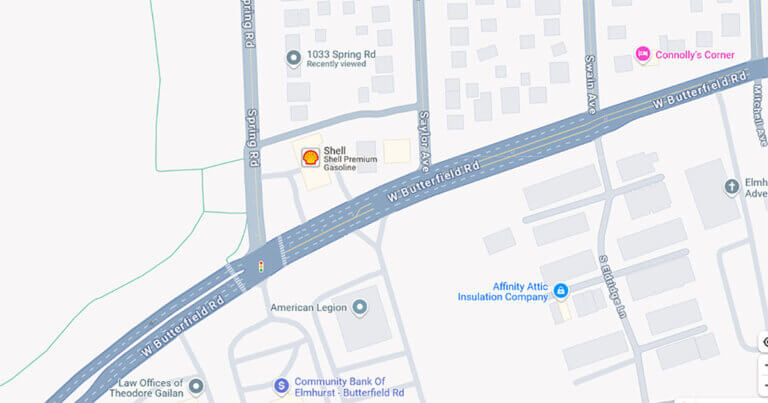
In my opinion, the local hospital of the future will be an ED, OR and ICU with a birthing center attached. A regional medical center will be within driving distance for urgent and elective care. Highly specialized national centers will serve as focus factories for sophisticated medical and surgical care, each serving patients from larger geographic areas, even from across the nation. Cancer surgery, joint replacements, open heart surgery, and other major non-emergency care and surgery at these focus factories will deliver higher quality more efficiently. As noted in Part 1, outcomes are objectively better at institutions focused on a limited number of conditions. [6]
Although this plan might sound exotic, other nations around the world already benefit with specialized, nonredundant hospitals. [7] And global competition is real. The U.S. won’t dominate high-end specialty care like it did in the 1900s. By the end of this century it will be a tripolar world shared between the U.S., China and India. Redistributing resources in America from less efficient healthcare to education, infrastructure, environment, and other worthwhile endeavors will help everyone. [8]
Outpatient care will continue the migration to virtual. Online shopping initially seemed exotic, but now packages arrive daily delivered to homes by a fleet of small vans. And as much as one pines for the old days with a personal intimate relationship with a caregiver, the power of quick access to accurate care will overcome nostalgia. Dr. Marcus Welby will be a distant memory. Consider the profound change from working five days a week in a physical office to the current geographically agnostic 24/7 virtual business community. Formerly successful commercial real estate owners are repurposing their now half-empty buildings.
When will the economics mandate a change? With a slower evolution, the existing systems have a chance to accommodate. A rapid and severe economic downturn is more likely to stimulate a quicker move. Costs matter, particularly as resources become more limited.
Medically self-insured employers like Walmart are already leading the way. Change is happening with younger patients sorting themselves out by going to walk-in clinics in big box chain stores and older folks seeking specialized care from major national systems. As outcomes improve and receive wider recognition, these positive changes will accelerate, creating a “flywheel effect.”
The End Game
 Like it or not, sooner or later as a patient or provider we will transform. Understanding the need to change along with better outcomes for patients, who everyone is trying to serve, should improve provider satisfaction.
Like it or not, sooner or later as a patient or provider we will transform. Understanding the need to change along with better outcomes for patients, who everyone is trying to serve, should improve provider satisfaction.
Subsequently, costs will drop, productivity will increase, and precious resources redirect to preventing illness and improving quality of life. Helping everyone live a longer, happier, and healthier life is an achievable goal. Healthcare systems can and should lead the transformation.
Sources
- “Life Expectancy in the U.S. Dropped for the Second Year in a Row in 2021,” National Center for Health Statistics, Centers for Health Statistics.
- “Inside Costa Rica’s Healthcare Success Story,” Harvard T. H. Chan School of Public Health, January 27, 2023.
- Exploring why Costa Rica outperforms the United States in life expectancy: A tale of two inequality gradients,” by Luis Rosero-Bixby and William Dow, PNAS, January 4, 2016.
- “Medicare Guidance for Mid-Level Providers,” by Advize, August 25, 2015.
- “Walmart Rolls Out Centers of Excellence Program,” by Chris Anderson, Healthcare Finance, November 6, 2012.
- “Why Shouldice?” Shouldice Hernia Hospital website.
- “Relationship between hospital specialization and health outcomes in patients with nonsurgical spinal joint disease in South Korea: A nationwide evidence-based study using national health insurance data,” by Boyoung Jung, Jiyoon Yeo, Sun Jung Kim, and In-Hyuk Ha, National Library of Medicine, August 13, 2021.
- “Tri-Polar World: India, China, and the United States in the 21st Century,” Carnegie Endowment for International Peace, February 9, 2011.