August 24, 2022
The Cost of Coding Is Killing Us
I’m fairly confident that no other industry spends more to bill and collect money from its customers than the healthcare industry. Someday, someone smart will attach a dollar figure to that statement by adding up the annual revenue generated by all of the healthcare revenue cycle management vendors out there with the annual revenue cycle budgets of hospitals, health systems and medical practices.
The number would be huge.
Also huge would be the list of reasons why hospitals, health systems and physicians spend so much on revenue cycle management in order to collect every dime payers and patients owe them for services.
A new study in Health Affairs points to one of those reasons: coding. Our current system in the U.S. of assigning billing codes to everything a provider does to a patient during an episode of care ultimately is making revenue cycle management specifically and healthcare services generally more expensive.
Coding, of course, is an appendage of fee-for-service payment systems that generates more revenue for providers by enabling them to charge for care on an itemized basis as opposed to one all-inclusive bill for everything. The more you dice up an episode of care, the more all those little pieces can add up.
Almost as if to prove the point, it took 12 researchers — 12! — from such vaunted educational institutions as Duke, Harvard, Stanford, Erasmus University and the University of Toronto to do this study, which you can download here.
The dozen researchers compared the cost of billing and insurance-related tasks, or BIR, in six countries: Australia, Canada, Germany, The Netherlands, Singapore and the U.S. They selected one representative site in each of the six countries and measured the time spent on four different BIR tasks in the order that they typically happen in the revenue cycle in each country:
- Eligibility
- Coding
- Submission
- Rework
They then calculated the cost per minute of doing each BIR task based on the type of personnel required to perform it and came up with a BIR cost in 2020 U.S. dollars for different types of medical bills.
The highest BIR cost was $215.10 for an inpatient surgical bill in the U.S. The lowest BIR cost was $5.80 for an inpatient nonsurgical bill in Canada.
Then the researchers broke down BIR costs for each type of medical bill by task. The biggest contributor to BIR costs in Australia, The Netherlands and, especially the U.S., was coding. In the U.S, $172.40 of the $215.10 BIR cost for that inpatient surgical bill — or 80.1 percent — went for coding. Coding ate up 71.2 percent of the BIR costs in Australia and 48.6 percent of the BIR cost in The Netherlands.
Stating the obvious, the researchers said, “We observed that high U.S. (BIR) costs are caused primarily by expensive and extensive coding activities.”
Further: “In the U.S., billing procedures often require providers to carefully document patient conditions and diagnoses to justify treatment and payment, and sophisticated coders then translate the diagnoses and service codes into billing codes (often manipulated to enhance revenue).” Emphasis added so you don’t miss the researchers saying the quiet part outloud.
As David Johnson, founder and CEO of 4sight Health likes to say, the smartest people in healthcare work in the revenue cycle department because it takes the biggest brains to maximize revenue from a single episode of patient care.
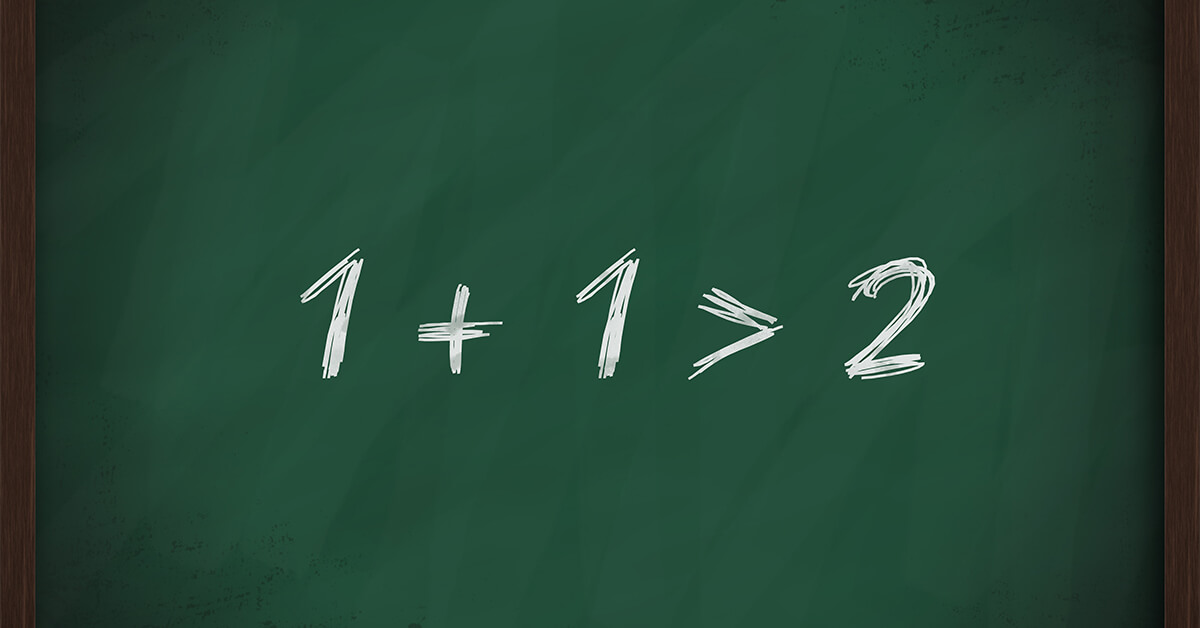
The study results also reveal to me another reason why it’s been so difficult to wean providers off fee-for-service payments and on to value-based care and alternative payment models. Providers can play with FFS codes to make more money. Kind of like the multi-part formulas that local taxing authorities use to calculate your property taxes. Change a number here and your property taxes go up even if the value of your property went down.
We need a healthcare billing system that works for customers, not for providers.
Thanks for reading.
To learn more on this topic, please read:





