January 9, 2020
Unrelenting Margin Pressures: Overcoming Healthcare’s Softening Revenues and Rising Expenses
Key Takeaways:
- Despite favorable rating agency outlooks, the 2020s promise to be healthcare’s most turbulent decade since the 1990s.
- It’s been a great 20-year run for the healthcare industry, but business as usual for hospitals and health systems is no longer a viable option.
- 5 key pressure points are driving down margins.
- Health systems must take 4 steps to relieve margin pressure.
- The time for change is now. More than innovation, execution will differentiate winners from losers.
In mid-December, Moody’s Investor Services and Fitch Ratings upgraded their outlooks for U.S. nonprofit health systems from negative to stable for 2020.[1] Standard & Poor’s, the third major rating agency, will issue its 2020 sector outlook later this month. In all likelihood, S&P will affirm its stable 2019 outlook.
The rating agencies cited more favorable payment rates, higher volumes, greater market concentration and stronger balance sheet ratios in revising their 2020 outlooks. These positive near-term developments should not fool health system leaders.
A host of market-driven and regulatory forces are fundamentally challenging traditional acute care operating models. These include a higher governmental payer mix, more discerning commercial buyers, more risk-based contracting, new competitors, changing consumer behaviors, and a dramatically shifting regulatory environment.
Together, these forces will make the coming decade the most challenging for hospitals and health systems since the 1990s. Unlike the 1990s, the solutions needed to meet current market challenges will require dramatic improvements in operating efficiency, and fundamental changes to health system business models.
Enlightened health system leaders will use this “calm before the storm” period to reposition their companies so they can compete more effectively by delivering higher value care services.
Despite favorable rating agency outlooks, the 2020s promise to be healthcare’s most turbulent decade since the 1990s.
The Bond Rating Fallacy
Unlike for-profit companies, nonprofit health systems operate for their communities’ benefit. Nonprofit companies cannot access equity funding or distribute earnings to shareholders. They fund investments through operating cash flows, debt, investments and charitable contributions.
As a consequence, nonprofit health systems that actively raise debt in the capital markets carry high levels of cash and investments on their balance sheets. Strong balance sheets lead to higher bond ratings and lower interest rates. In its report, Fitch noted that balance sheet ratios are at their highest levels since the 2007 Great Recession.
By design, rating agencies evaluate the individual credit standing of nonprofit hospitals and health systems based on their ability to repay indebtedness, not their longer-term competitive positioning. Their horizon is short, just two years.
Strong balance sheets combined with increasing near-term service payments justify their collective assessment that the nonprofit healthcare industry’s outlook is stable. Bond payments are secure for now. Immediate bond defaults are not a credit concern.
Given their robust bond ratings, nonprofit health systems appear stronger than they really are. They operate capital-intensive, low-margin facilities that require highly skilled workers. They are vulnerable to new, more efficient competitors that deliver better outcomes at lower costs.
Dynamic forces are reshaping the healthcare industry’s supply-demand relationships in ways that fundamentally challenge traditional health system business models. This happened once before, during the 1990s, and forced many hospitals and health systems to their knees.
It is instructive to revisit the 1990s to examine how hospitals stumbled and then recovered. Beginning in the early 2000s, a massive infusion of new provider revenues triggered industry resurgence. History will not repeat itself.
Throwback to 1999
During the 1990s, healthcare expenditures remained relatively flat. For the first and only time since World War II, healthcare expenditures grew at the same rate throughout the decade as the overall economy.
Throughout the 1990s, a mix of forces slowed the industry’s previously high growth rate. The most important was the emergence of widespread managed care contracting through health maintenance organizations (HMOs). HMOs received fixed monthly payments to manage the care of their subscribers.
HMOs employed primary care physicians (PCPs) as gatekeepers to guide access to acute treatments. While this approach did reduce unnecessary utilization, it also incentivized PCPs to restrict access to necessary care and often forced members to receive care at lower-cost institutions.
As a result, hospitals and health systems saw their revenues and profits diminish. In response, many formed their own insurance companies and/or employed physicians, notably PCPs, to increase their referral volume. In theory, this vertical integration enabled health systems to control a higher percentage of healthcare expenditure. Most of these investments, however, proved disastrous. Hospitals and health systems deployed excessive capital to buy physician practices when they lacked the capabilities to manage the utilization of those practices. The passage of the Balanced Budget Act in 1997, which cut governmental payments to hospitals, amplified operating pressures.
By the late 1990s, many providers were bleeding red ink. Moody’s coined the term “century club” to describe health systems with operating losses exceeding $100 million. Bond rating downgrades exceeded upgrades by a wide margin. Some organizations risked insolvency.
It’s been a great 20-year run for the healthcare industry, but business as usual for hospitals and health systems is no longer a viable option.
When their future appeared at its most bleak, market dynamics for hospitals suddenly improved. Consumers seethed with anger over HMOs’ lengthy, bureaucratic and depersonalized care denials. Most HMOs folded. At the same time, federal spending restrictions imposed by Congress in 1990 and 1997 expired. With the federal budget in surplus for the first time in decades, the Centers for Medicare and Medicaid Services (CMS) began to deficit-fund healthcare expenditures.
As the new millennium unfolded, robust fee-for-service payments propelled hospital revenues and profitability upward. Increasing cash flow expanded providers’ capital capacity and fueled massive investment in new acute care facilities to meet pent-up demand. Low interest rates and synthetic debt instruments turbocharged borrowing and capital investment. Happy days were there again.
In 2009, Congress passed the Health Information Technology for Economic and Clinical Health (HITECH) Act that included funding for electronic health records (EHRs). Since 2011, the federal government has invested almost $40 billion in EHRs for doctors and hospitals.[2] Prior to HITECH, over 90% of hospitals primarily used paper health records. Today, fewer than 5% do.[3]
The passage of the Affordable Care Act (ACA) in 2010 was another watershed event. The ACA expanded access to healthcare services and pumped billions of dollars in new revenue into the U.S. healthcare system but failed to control healthcare spending.
It’s been a great 20-year run for the healthcare industry. Healthcare expenditures as a percentage of GDP have grown from 13% in 1999 to 18% today.[4] They show no signs of slowing. CMS projects that national healthcare expenditures will increase 5.5% annually through 2027, growing from $3.8 trillion in 2019 to almost $6 trillion by 2027.[5]
Frustration with the industry’s inability to control costs, however, is mounting. Government deficits are at record levels driven increasingly by uncontrolled healthcare expenditure. Commercial insurance premiums have grown at a rate three times greater than the consumer price index (CPI) since 1999. The financial fallout from medical bills, including lost wages, is the leading cause of personal bankruptcies.
Hospitals and doctors consume the majority of healthcare spending.[6] Therefore, it should come as no surprise that the American society is demanding greater value from providers. They are manifesting this desire through a powerful blend of market-driven and regulatory reforms.
Business as usual for hospitals and health systems is no longer a viable option.

Revolutionary Forces Driving Margin Pressure
Healthcare’s good times cannot last forever. Similar to what happened in the 1990s, healthcare companies are consolidating and repositioning in response to market and regulatory forces. Large health systems emerged in the late 1990s to strengthen their negotiating leverage with payers and achieve economies of scale.
Initially, most health systems were horizontally integrated hospital holding companies. As they mature, health systems are striving to become vertically integrated operating companies that can accommodate full-risk contracting. This is very much a work in progress. It represents a strategic response to marketplace demands for greater transparency, better outcomes and value-based care delivery.
From a macro perspective, the industry needs to rationalize and/or repurpose the glut of acute care facilities that have materialized over the last two decades. Overinvestment in acute and specialty care services has driven healthcare payments into the stratosphere and minimized the role primary care plays in disease prevention, overall health promotion and care management.
Both the marketplace and government regulators see opportunity to improve the efficiency and effectiveness of healthcare delivery through targeted initiatives. They’re making their presence felt. Surveying the competitive landscape, health system leaders are confronting the following forces that are reshaping market demand for healthcare services and rendering many of health system’s once-profitable business practices as noncompetitive.
Shifting Payer Mix: Ten thousand baby boomers are aging into Medicare every day.[7] Most are shifting out of higher-paying commercial health insurance into lower-paying government-funded programs. Moreover, new Medicare beneficiaries are rapidly enrolling in Medicare Advantage (MA) plans that force providers to take on more risk than traditional Medicare. Shifting payer dynamics will reduce both revenues per case and impact patient utilization of hospital services as Medicare coverage spreads and MA plans manage utilization.
More Disciplined Purchasing: Corporate buyers are becoming more sophisticated and disciplined buyers of healthcare services. Some, like Walmart and Comcast, have reconfigured the HMO gatekeeper model through third-party partnerships (e.g., Grand Rounds for Walmart[8] and Crossover Health for Comcast[9]) to manage their employees’ primary care and referral needs. Since self-insured corporations bear their employees’ healthcare costs and want healthier, more productive employees, their gatekeeper initiatives focus on health promotion, early diagnosis and active care management, opposed to care denials.
Other corporate and governmental buyers are using full risk bundled contracts with preselected providers to improve outcomes and reduce costs. These more disciplined buying practices require all healthcare providers to be more transparent and accountable for their pricing, outcomes and customer experience.
Changing Consumer Behaviors: The CDC now estimates that 47% of Americans with private health insurance are now enrolled in high deductible health plans (HDHP)[10] with an average family deductible of approximately $5,000.[11] These consumers are becoming more cost conscious when evaluating their care options, especially when offered reference prices.12 Since most HDHP enrollees don’t meet their annual deductible, many choose to negotiate cash prices for procedures with providers when they require elective procedures.
Moreover, new technologies and apps are emerging to support consumers who want to shop for healthcare services. With more skin in the game and better tools, increasing numbers of consumers are exercising control over their healthcare purchasing. Like consumers in other industries, healthcare consumers are very price conscious. When it’s their money, they won’t pay extra for routine care.
New Competitors: Most healthcare services are routine and vulnerable to commodity pricing. Record levels of venture and private equity funding are flowing into healthcare to build companies that offer routine care services at much lower price points. These companies target the inefficient components of the massive healthcare ecosystem and develop business models that offer high value to purchasers of those services.
New-age healthcare companies are technology savvy, asset light and consumer oriented. They deliver targeted services from urgent care to MRIs to colonoscopies to women’s health services, conveniently and with transparent pricing. Market by market, procedure by procedure, diagnostic test by diagnostic test, these companies are increasing margin pressure on traditional providers by offering kinder, smarter, more affordable and more convenient healthcare services.
Dramatically Shifting Regulatory Environment: As an industry, healthcare has influenced the design of regulatory and legislative policies and practices by lobbying elected officials and government agencies. This is becoming harder to do. Current HHS leadership is taking aggressive measures to improve data and price transparency, level competition, and promote value-based purchasing.
On the payment front, CMS is moving towards direct contracting and payment programs that incentivize providers to accept downside frisk for the care they provide. New regulatory proposals seek to improve data interoperability and access, make commercial payers and providers reveal their negotiated payment rates for specific procedures and force site-neutral payment for healthcare service — in part by eliminating higher payments to hospital-based providers.
In the aggregate, these pro-market policies and regulations aim to hold providers, particularly hospitals, more accountable for their performance and outcomes.
The cumulative and compounding effect of these five forces places an enormous strain on those health system business models that optimize revenues at the expense of value-based care delivery. Health systems will face “death by a thousand cuts” as the marketplace finds more efficient ways to deliver appropriate, holistic and affordable healthcare services that are convenient, accessible, reliable and evidenced-based.
Providers Respond
In Ernest Hemingway’s The Sun Also Rises, war veteran Bill Gorton asks his buddy Mike Campbell how he went bankrupt. Mike responds, “Two ways. Gradually and then suddenly.” This is the defining pattern of disruptive change. It builds slowly and then overwhelms incumbents when they no longer have the capacity to respond.
The most important step for health system leaders now is to understand and appreciate the virulence of the forces aligning to revolutionize healthcare service delivery. Given the size and strength of the nation’s health systems, it is easy to be overconfident, even complacent, and believe that business as usual is a sustainable strategy.
The time for change is now. Buyers and consumers of healthcare services are demanding both higher value healthcare services and greater access to essential, but low-paying primary care services (e.g., chronic disease management and behavioral health). Accommodating these market preferences will fundamentally reshape the industry’s supply-demand relationships and its allocation of resources. Many hospitals will close.
To improve profitability and increase organizational viability, health system leaders must simultaneously run their acute care operations more efficiently while proactively reconfiguring service delivery platforms. They must deliver more convenient, lower-cost services that consumers increasingly demand. It’s a tricky balancing act with little room for error and no time to waste. Here are a few strategies with the biggest potential to relieve margin pressure.
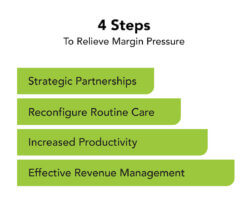
Strategic Partnerships: An African proverb observes that “If you want to go faster, go alone. If you want to go farther, go together.” Across industries, businesses are reconfiguring themselves to operate seamless Amazon-like platforms that deliver great products and services tailored to customer needs.
No company excels at everything. Strategic partnerships with companies that can deliver vital services under a unified brand are essential to health systems’ long-term sustainability. For example, health systems lack the retail expertise to operate profitable and consumer-friendly urgent care centers. Consequently, some health systems are operating urgent care centers with strategic partners (e.g. Hartford HealthCare with GoHealth) that have mastered that business. These types of strategic partnerships can go a long way together.
Reconfigure Routine Care: The majority of healthcare services are episodic, routine and achieve predictable results. They are essentially retail offerings that lend themselves to high volume, low margin delivery platforms that deliver consistent quality and convenience to consumers. Continuing to expect buyers to pay premium prices for routine services is wishful thinking.
The realistic alternative for health systems is to shift routine care to lower cost, more convenient facilities that can be profitable while receiving commodity-like payment for services rendered. Retail businesses are competitive, lean and customer focused. Health systems have little understanding of or experience in operating retail enterprises, so succeeding as retail service providers will be difficult, if not impossible, for most.
Increased Productivity: “Better, faster, cheaper” has never had more applicability in healthcare than it does now. As in other industries, to be competitive health systems must understand costs, eliminate waste and manage supplies. As payment aligns with cost, effectively managing expenses will translate into higher profits. As Ben Franklin observed almost 300 years ago in Poor Richard’s Almanac, “A penny saved is a penny earned.”
Effective Revenue Management: Channeling Franklin, it is also true that a penny captured is a penny earned. Fee-for-service is not disappearing. Neither are co-pays and deductibles, in fact they are increasing. Risk-based agreements are expanding across many markets. Providers will need to be effective at managing a diverse spectrum of payment models. Digitizing claims data, hyper automation, consumer digital engagement and predictive analytics are examples of the essential capabilities needed to optimize a diverse and complex revenue mix. Every new dollar realized goes straight to the bottom line.
Each of these practical strategies will contribute to a health system’s ability to deliver high-value services at competitive prices. In this sense, these are tactical rather than pathbreaking initiatives. More than innovation, execution will differentiate winners from losers. Health systems that fail to “gradually” transition to customer-centric service platforms will “suddenly” discover that they’ve lost market relevance.
Conclusion: Waves and Tides
Every sailor knows that waves move independently from tides. Health system leaders must not mistake today’s short-term revenue gains as a signal that they’ve weathered the disruptive storms confronting the industry. The tide is turning on centralized, expensive and fragmented business models that deliver suboptimal outcomes.
The margin pressures health systems confront are real and not going away. Doubling down on existing business practices is a recipe for failure. Embracing practical strategies that deliver optimal outcomes is the only way to relieve the pressure. Unlike the late 1990s, there are no budget surpluses or pent-up pockets of demand available to rescue providers from themselves.
Instead, health systems must radically reconfigure their care delivery offerings to meet customer service demands and price points. Achieving this level of operating proficiency will require robust digital platforms that frame relevant financial and operational data in real time; strategic partnerships that enhance service provision and create value; and user-friendly technologies that enhance outcomes and consumer experience. Consistency, convenience and cost will differentiate market winners and losers.
A new wave of revolutionary upstart and incumbent healthcare companies is riding the disruptive tide. These companies are shifting resources out of acute and specialty care into better care management, behavioral health and health promotion. They’re aligning their services with consumers’ needs, wants and desires. They’ll win by delivering the right care at the right time in the right places at the right prices.
Comments, Questions, Want to Debate?
Reach out to David.Johnson@4sighthealth.com or JeffJones@ConiferHealth.com
Sources
- https://www.healthcaredive.com/news/nonprofit-hospitals-get-bump-in-moodys-ratings-for-2020/568739/
- https://ehrintelligence.com/news/ehr-use-high-administrative-burden-driving-healthcare-spending
- https://dashboard.healthit.gov/quickstats/pages/FIG-Hospital-EHR-Adoption.php
- https://www.cms.gov/Research-Statistics-Data-and-Systems/Statistics-Trends-and-Reports/NationalHealthExpendData/ NationalHealthAccountsHistorical
- https://www.cms.gov/Research-Statistics-Data-and-Systems/Statistics-Trends-and-Reports/NationalHealthExpendData/ Downloads/ForecastSummary.pdf
- https://www.cms.gov/files/document/highlights.pdf
- https://www.forbes.com/sites/brucejapsen/2019/02/20/baby-boomers-to-push-u-s-health-spending-to-6-trillion-by2027/#6fd6a736b2d5
- https://medcitynews.com/2019/10/care-coordination-firm-grand-rounds-embraces-larger-role-with-walmart/
- https://crossoverhealth.com/press/crossover-health-launches-connected-system-of-health/
- https://www.cdc.gov/nchs/data/nhis/earlyrelease/Insur201808.pdf
- https://www.kff.org/report-section/ehbs-2019-section-8-high-deductible-health-plans-with-savings-option/
- https://www.mitpressjournals.org/doi/full/10.1162/ajhe_a_00118
Co-author
 Jeff Jones serves as Chief Commercial and Strategy Officer for Conifer Health Solutions. In this role, he defines the strategic direction for Conifer including the enterprise strategy, strategic partnerships, leads all commercial activities, heads client service and delivery, owns brand, marketing and go to market strategy, and directs new solution innovation. Jeff joined Conifer’s Executive Leadership Team in September 2019 bringing with him over 30 years of industry experience. Jeff’s experience in both the healthcare and technology industries coupled with his demonstrated track record partnering with health systems, academic medical centers, specialized providers, medical groups and health technology companies allows him to bring unparalleled insights into Conifer’s overall business.
Jeff Jones serves as Chief Commercial and Strategy Officer for Conifer Health Solutions. In this role, he defines the strategic direction for Conifer including the enterprise strategy, strategic partnerships, leads all commercial activities, heads client service and delivery, owns brand, marketing and go to market strategy, and directs new solution innovation. Jeff joined Conifer’s Executive Leadership Team in September 2019 bringing with him over 30 years of industry experience. Jeff’s experience in both the healthcare and technology industries coupled with his demonstrated track record partnering with health systems, academic medical centers, specialized providers, medical groups and health technology companies allows him to bring unparalleled insights into Conifer’s overall business.






