March 21, 2019
Why Healthcare is Spinning Its VBR Wheels

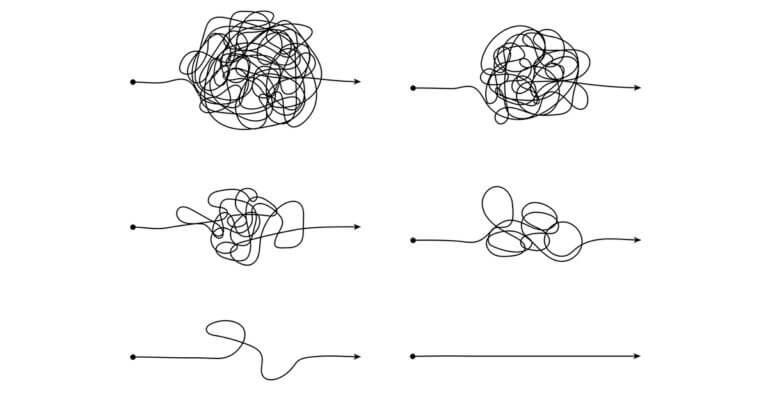
It’s like preparing and serving a seven-course meal that your biggest customer ordered only to have the entire menu change between the salad and the main course. That’s what it must feel like for hospitals and doctors dealing with the ever-changing value-based reimbursement programs from Medicare.
That thought came to mind when reading the Medicare Payment Advisory Commission’s latest annual March report to Congress. The 531-page tome makes all kinds of recommendations to the federal legislative branch on how to improve the government’s health insurance program for seniors.
About 20 pages in the report are devoted to MedPAC’s recommendation to replace four Medicare VBR programs with a new one called the hospital value incentive program, or HVIP. (For those who want to skip to that part, it’s Chapter 15.)
The four VBR programs that MedPAC wants Congress to dump are the:
- Hospital Inpatient Quality Reporting Program, or IQRP
- Hospital Readmissions Reduction Program, or HRRP
- Hospital Value-based Purchasing Program, or VBP
- Hospital-Acquired Condition Reduction Program, or HACRP
Specifically, MedPAC wants Congress to sunset the IQRP and combine HRRP, VBP and HACRP into one program, HVIP. Under HVIP, Medicare would score hospitals based on how well they score on performance measures in five categories:
- Readmissions
- Mortality
- Medicare spending per beneficiary
- Patient experience
- HAC rate
Specifically, MedPAC wants Congress to sunset the IQRP and combine HRRP, VBP and HACRP into one program, HVIP. Under HVIP, Medicare would score hospitals based on how well they score on performance measures in five categories:
- Readmissions
- Mortality
- Medicare spending per beneficiary
- Patient experience
- HAC rate
Medicare would score all hospitals the same way but would divide hospitals into 10 “peer groups” that would adjust their payments based on how well they scored against hospitals with similar patients.
Why get rid of IQRP and merge HRRP, VBP and HACRP into HVIP (other than to make editors everywhere update their healthcare acronym style sheets)?
In a press release, MedPAC said, “Despite their successes, the designs of the current hospital quality payment programs are complex, in some instances duplicative, and send different performance signals to hospitals.”
In the report, MedPAC said the change would reduce the quality measure reporting burden on providers and make Medicare payment adjustments “more equitable” among hospitals that treat different patient populations with different risk factors.
And how would this help patients? “Beneficiaries may benefit from hospitals’ enhanced incentives to improve the quality of care they provide,” MedPAC said with apparent fingers crossed. (Italics added.)
I’m all for efficiency and equity if it leads to better outcomes at less cost for patients. Maybe that’s what would happen if Congress did what MedPAC wants. But I also think that it’s the constant change in how Medicare and other payers judge provider performance that has VBR losing momentum in the industry. Why invest in the people, technologies and other resources when you know the rules will change?
The latest surveys to note the VBR slippage come from Numerof & Associates in its four annual State of Population Health survey and from Change Healthcare and the Healthcare Executive Group (HCEG) in their ninth annual Industry Pulse Survey.
Some 528 healthcare c-suite executives took this year’s State of Population Health survey from Numerof. Two-thirds said their organizations have 20 percent or less than their revenue coming from risk-based agreements with payers. They had predicted much more in earlier iterations of the survey.
“Uncertainty regarding which direction Washington will go has resulted in many hospital administrators pushing ‘pause’ on their population health efforts,” the report said.
Some 185 healthcare leaders took this year’s Industry Pulse Survey from Change Healthcare and HCEG. Nearly 40 percent said that they don’t expect the majority of their value-based contracts to feature both upside and downside risk for another three to five years. The lack of standardized quality and outcomes measures was the top reason cited by the respondents for the slow progress.
“Healthcare seems to be perpetually stuck at being three to five years away from adopting shared-risk value-based contracts,” the report said.
In an earlier post, “The Slow Road to Value-Based Care” we noted other studies, reports and surveys that have shown that the pace of VBR adoption is slowing to a crawl.
Patients deserve better. VBR adoption should be accelerating. Like anything in business, if the rules get too complicated or keep changing, innovation bogs down. It’s time to make VBR simple, meaningful and predictable.
David Burda is a columnist for 4sight Health and news editor of 4sight Friday, our weekly newsletter. Follow Burda on Twitter @DavidRBurda and on LinkedIn. Read his bio here.